AI in Medicine and Healthcare
Artificial Intelligence (AI) is revolutionizing medicine and healthcare by enhancing diagnostics, improving patient care, and streamlining medical operations. From predictive analytics to personalized treatment plans, AI is driving innovation and efficiency in the healthcare industry.
AI (Artificial Intelligence) is rapidly transforming medicine and healthcare worldwide. With an estimated 4.5 billion people lacking access to essential healthcare and a projected shortfall of 11 million health workers by 2030, AI offers tools to improve efficiency, extend reach, and close gaps in care.
AI digital health solutions hold the potential to enhance efficiency, reduce costs and improve health outcomes globally.
— World Economic Forum (WEF)
In practice, AI-driven software is already outperforming humans in some diagnostic tasks. For example, an AI trained on stroke patient scans was twice as accurate as expert clinicians at identifying and dating brain strokes.
- 1. AI-Powered Medical Imaging & Diagnostics
- 2. Clinical Decision Support & Patient Management
- 3. Administrative & Operational Efficiency
- 4. Research, Drug Development & Genomics
- 5. Global Health & Traditional Medicine
- 6. Key Benefits of AI in Healthcare
- 7. Challenges, Risks & Ethics
- 8. Regulation & Governance
- 9. Future Outlook
- 10. Top AI Tools in Healthcare
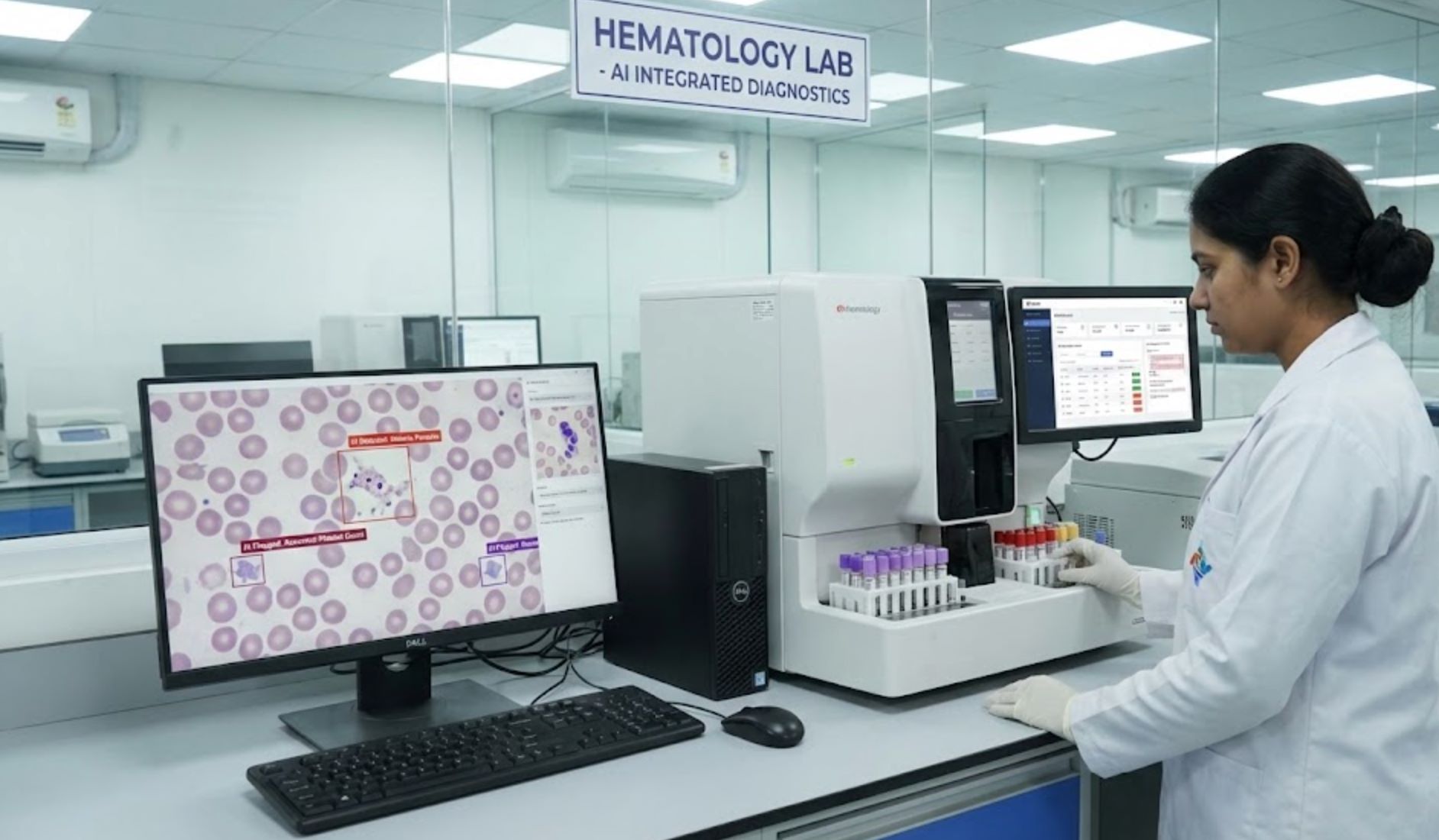
AI-Powered Medical Imaging & Diagnostics
AI is already reading medical images (like CT scans and X-rays) faster than people. AI tools can spot abnormalities in minutes — from stroke scans to broken bones — helping doctors diagnose faster and more accurately.
Simple imaging tasks like finding fractures are ideal for AI: urgent-care doctors miss up to 10% of breaks, but AI review can flag these early. By acting as a "second pair of eyes," AI helps avoid missed diagnoses and unnecessary tests, potentially improving outcomes and lowering costs.

Clinical Decision Support & Patient Management
AI is also boosting clinical decision support and patient management. Advanced algorithms can analyze patient data to guide care.
Early Disease Detection
AI models can detect signatures of diseases years before symptoms appear:
- Alzheimer's prediction
- Kidney disease forecasting
- Cancer risk assessment
Clinical Chatbots & LLMs
Specialized systems combining LLMs with medical databases:
- 58% useful clinical answers (US study)
- Retrieval-augmented generation
- Digital assistant capabilities
Digital Patient Platforms
Digital patient platforms are another growth area. The Huma platform, for example, uses AI-driven monitoring and triage to reduce hospital readmissions by 30% and cut clinician review time by up to 40%.
Remote monitoring devices (like wearables and smart apps) use AI to track vitals continuously — predicting heart rhythm issues or oxygen levels in real-time — giving doctors data to intervene early.
Administrative & Operational Efficiency
In administrative and operational tasks, AI is easing workloads. Major tech companies now offer "AI co-pilots" for healthcare:
Dragon Medical One
Google AI Tools
AI Adoption Statistics
Surveys show physicians are already using AI for routine documentation and translation services. In a 2024 AMA survey, 66% of doctors reported using AI tools (up from 38% in 2023) for tasks like charting, coding, care plans or even preliminary diagnoses.
Research, Drug Development & Genomics
Beyond the clinic, AI is reshaping medical research and drug development. AI accelerates drug discovery by predicting how molecules behave, saving years of lab work.
AlphaFold
Cancer Prediction
TB Diagnosis
Genomics and personalized medicine benefit too: AI can analyze vast genetic data to tailor treatments to individual patients. In oncology, Mayo Clinic researchers use AI on imaging (like CT scans) to predict pancreatic cancer 16 months before clinical diagnosis — potentially enabling earlier interventions for a disease with otherwise very poor survival rates.

Global Health & Traditional Medicine
AI's impact extends worldwide. In low-resource settings, smartphone AI can bridge care gaps: for example, an AI-powered ECG app flags heart disease risks, even where cardiologists are scarce.
- India: AI-driven digital library of Ayurvedic texts
- Ghana & Korea: AI classification of medicinal plants
- WHO Agenda: Making traditional medicine more accessible globally
These efforts — part of WHO's agenda — aim to make traditional medicine more accessible globally without exploiting local communities. Overall, AI is seen as a way to help achieve universal health coverage (a UN goal by 2030) by extending services to remote or underserved areas.

Key Benefits of AI in Healthcare
Faster, More Accurate Diagnostics
AI can process images and data at scale, often catching what humans miss
Personalized Care
Algorithms tailor treatment plans from patient data (genetics, history, lifestyle)
Efficiency Gains
Automating paperwork and routine tasks reduces clinician burnout significantly
Cost Savings
McKinsey estimates AI could save hundreds of billions annually through improved productivity
Expanded Access
AI-driven telemedicine allows rural/poor regions to access expert-level screening
Better Outcomes
Patients benefit from improved health outcomes and lower healthcare costs
AI holds great promise for improving the delivery of healthcare and medicine worldwide.
— World Health Organization (WHO)

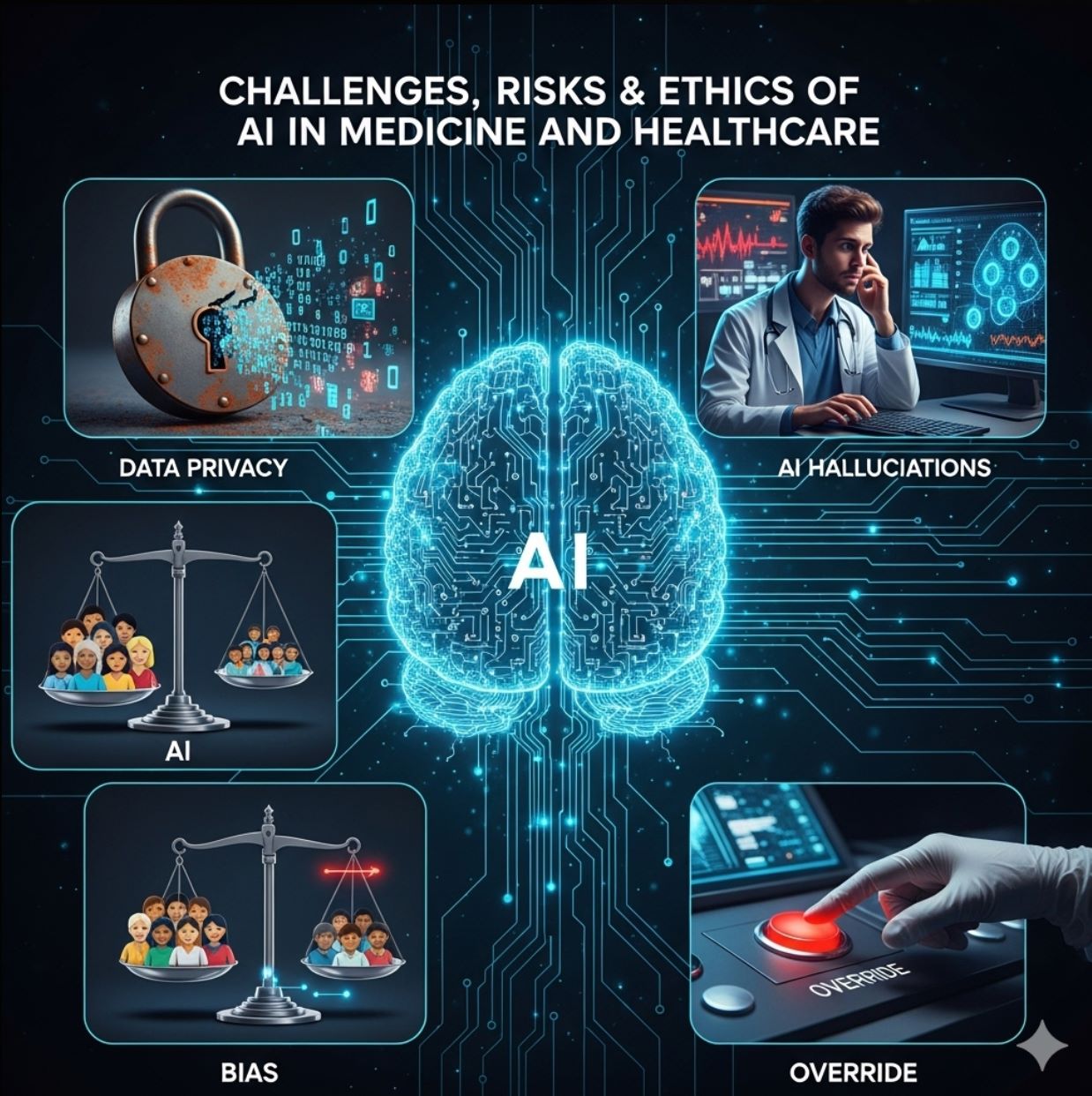
Challenges, Risks & Ethics
Despite promise, AI in healthcare faces serious challenges that must be addressed to ensure safe and equitable implementation.
Data Privacy & Security
Health data is highly sensitive, and poor de-identification can risk patient confidentiality. Robust security measures and compliance with regulations like HIPAA and GDPR are essential.
Bias in AI Models
If algorithms are trained on non-diverse data (for example, mostly on high-income country patients), they may perform poorly for others.
Clinician Trust & Training
Rapid deployment of AI without proper education can lead to misuse or errors. Healthcare professionals need comprehensive training to understand AI capabilities and limitations.
Users must understand and know how to mitigate AI's limitations.
— Oxford Ethicist
AI Hallucinations & Errors
AI systems (especially LLMs) can hallucinate — making up plausible-sounding but false medical information.
- OpenAI's Whisper occasionally invented details in transcriptions
- Popular LLMs often fail to give fully evidence-based medical answers
- Human oversight remains essential for all AI-generated medical content
WHO Ethical Principles for AI in Healthcare
Autonomy
Well-being & Safety
Transparency
Accountability
Equity
Sustainability
Regulation & Governance
Regulators worldwide are already stepping in to ensure AI healthcare systems meet safety and efficacy standards.
FDA Approach
- Fast-tracked 1,000+ AI-enabled medical devices
- January 2025: Comprehensive draft guidance for AI/ML software
- Covers entire lifecycle from design to post-market monitoring
- Addresses transparency and bias explicitly
- Drafting rules for AI in drug development
EU & UK Regulations
- EU AI Act (2024): Healthcare AI as "high-risk"
- Strict requirements for testing and documentation
- Mandatory human oversight for critical systems
- UK MHRA: Regulates AI medical devices under existing law
- Emphasis on clinical validation and safety
AI can improve the health of millions if used wisely, but it can also be misused and cause harm.
— Dr. Tedros Adhanom Ghebreyesus, WHO Director-General
Thus, international organizations call for guardrails that ensure any AI tool is safe, evidence-based, and equitable.

Future Outlook
Looking ahead, AI's role in healthcare will only grow. The future promises unprecedented integration of AI across all aspects of medical care, from prevention to treatment and beyond.
Advanced Generative AI
Generative AI (like advanced LLMs) will power more patient-facing apps and decision aids — as long as accuracy improves. Integration with electronic health records and genomics will create even more personalized care.
AI-Assisted Surgery
Robotics and AI-assisted surgeries will become commonplace in high-tech hospitals, offering precision and consistency beyond human capabilities.
Continuous Health Monitoring
Wearable sensors plus AI algorithms will continuously monitor health metrics, alerting patients and doctors to issues before emergencies occur.
Global AI Governance
Global initiatives (like the WEF's AI Governance Alliance) aim to coordinate responsible AI development across borders.
With cautious optimism, healthcare systems are beginning to embrace AI to achieve better health for more people — from smart diagnostics and streamlined clinics to breakthroughs in treatments and global health equity.

Top AI Tools in Healthcare
Ada Health
Application Information
| Developer | Ada Health GmbH, a Berlin-based health-technology company founded in 2011 by Claire Novorol, Martin Hirsch, and Daniel Nathrath |
| Supported Devices | Android (Google Play), iOS / iPhone (App Store), Web browser (ada.com) |
| Languages & Availability | Available in English, German, French, Spanish, Portuguese, Romanian, and Swahili. Used in over 148 countries worldwide |
| Pricing | Free for consumers. Enterprise and health system integrations available commercially |
What is Ada Health?
Ada is an AI-powered symptom assessment tool that helps users analyze their symptoms, receive possible condition suggestions, and get personalized guidance on next steps—whether that's self-care, scheduling a doctor visit, or seeking emergency care.
The platform combines a clinician-curated medical knowledge base with intelligent reasoning logic to deliver tailored follow-up questions and narrow down likely causes. Users can track symptom progression over time, export detailed reports, and use the insights to facilitate more informed discussions with healthcare providers.
How Ada Works: Clinical Rigor Meets AI
In the crowded digital health landscape, Ada distinguishes itself through clinical rigor, user safety, and a hybrid knowledge-and-reasoning approach—rather than relying solely on black-box machine learning algorithms.
The app's intelligent logic dynamically selects the next question based on your previous answers, optimizing for diagnostic clarity while minimizing user burden. You're guided through a conversation-like flow: starting with your primary symptom, then answering questions about onset, severity, duration, and related features. This interactive process helps Ada generate a ranked list of plausible diagnostic hypotheses alongside evidence-based triage advice.
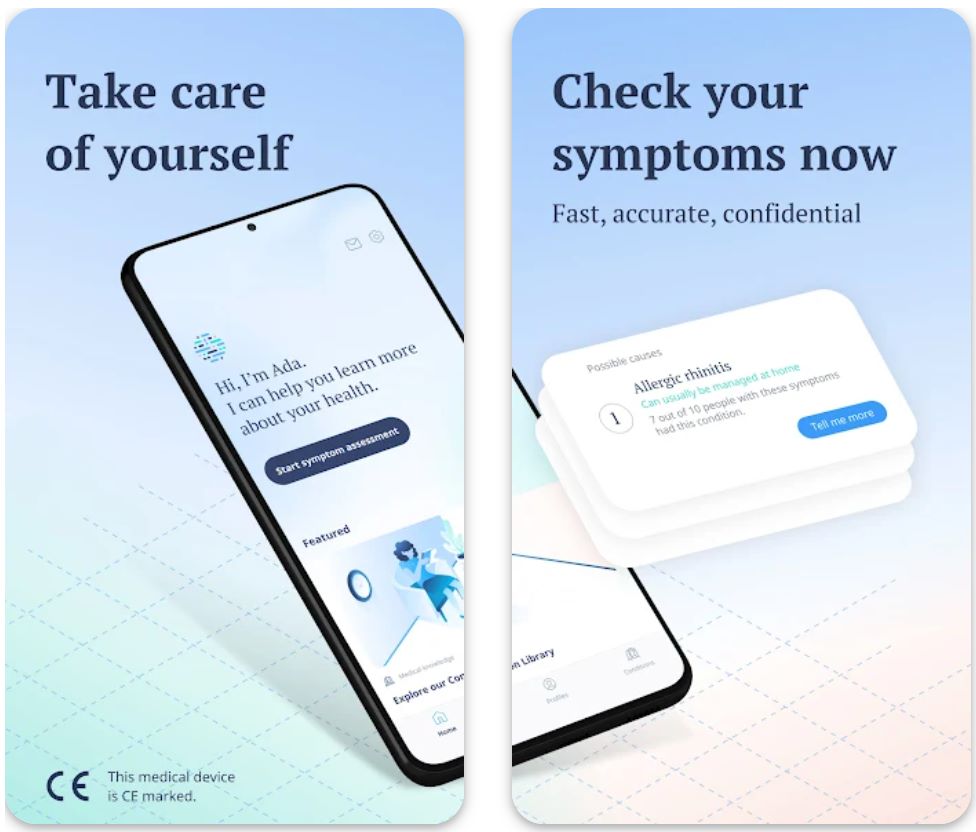
Key Features
Conversational interface with intelligent, guided questions that adapt based on your responses
Receive clear guidance on whether to self-care, schedule a doctor visit, or seek emergency care
Monitor symptom trends and changes to identify patterns and progression
Generate and share comprehensive PDF reports with your healthcare providers
In-app medical library with detailed condition explanations and health information
Create and manage profiles for family members to assess symptoms for others
Download or Access Link
How to Use Ada Health
Download Ada from Google Play Store, Apple App Store, or access directly via web browser at ada.com
Enter basic information including age, biological sex, and relevant medical history such as chronic conditions or medications
Select your primary symptom from the list (e.g., headache, cough, fever, fatigue)
Respond to Ada's intelligent questions about symptom duration, severity, location, and accompanying symptoms
View ranked list of possible conditions with detailed explanations and evidence-based triage advice
Log additional symptoms over days or weeks to monitor progression and identify patterns
Generate a comprehensive PDF summary to share with your physician for more informed consultations
Switch languages, manage multiple profiles, or adjust preferences in the settings menu
Important Limitations & Considerations
- Diagnostic and triage accuracy are probabilistic—Ada may misinterpret rare or complex medical cases
- Assessment quality depends on clear and complete user input; ambiguous answers may reduce accuracy
- Some features or data integrations may be restricted by region or regulatory approvals
- In emergencies or for serious symptoms, always seek immediate professional medical care
Frequently Asked Questions
Yes, Ada is classified as a CE-certified Class IIa medical device under EU regulations, meeting strict safety and performance standards for medical software.
Ada has completed millions of symptom assessments globally and is actively used in over 148 countries worldwide, making it one of the most widely adopted AI health companions.
In comparative clinical studies, Ada's top-3 diagnostic match rate was approximately 63%, and its triage recommendations aligned with physician judgment about 62% of the time. While impressive for an AI tool, it's designed to complement—not replace—professional medical evaluation.
No, the consumer symptom checker app is completely free for individual users. Ada also offers commercial enterprise integrations and health system partnerships for healthcare organizations.
Ada supports seven languages (English, German, French, Spanish, Portuguese, Romanian, and Swahili) and is available globally in many countries. However, specific language options and feature availability may vary by region due to regulatory requirements.
K Health
Application Information
| Author / Developer | K Health (formerly Kang Health), a privately held AI-powered healthcare company founded in 2016 in New York, USA. |
| Supported Devices | Android (Google Play), iOS / iPhone (App Store), Web browser interface via K Health's website |
| Languages / Countries | English (primary). Available in 48 U.S. states for virtual services with nationwide health system partnerships. |
| Pricing Model | Free symptom checker. Virtual visits with clinicians require payment (pay-per-visit or membership subscription). |
General Overview
K Health is a telehealth and AI-powered primary care platform that allows users to check symptoms, connect with healthcare providers, and manage care remotely.
The platform combines a symptom assessment engine—powered by data from millions of anonymized medical records—with live access to licensed clinicians. Users can receive diagnoses, prescriptions, advice for chronic condition management, and urgent care, all without needing to visit a clinic in person.
Detailed Introduction
In the competitive digital health arena, K Health positions itself as an AI-augmented primary care and urgent care solution targeted for consumers who want fast, affordable, and accessible medical care. The platform emphasizes virtual doctor visits, 24/7 care, symptom checking, telemedicine, and AI-powered health assistance.
The platform's hybrid model—symptom assessment followed by clinician consultation—aims to lower barriers to entry for healthcare. Its use of anonymized "people like you" treatment data helps personalize recommendations and differentiate it from simple symptom checkers. K Health's public content reinforces authority for health-related search queries through comprehensive FAQ, blog posts, symptom explanations, and educational resources.
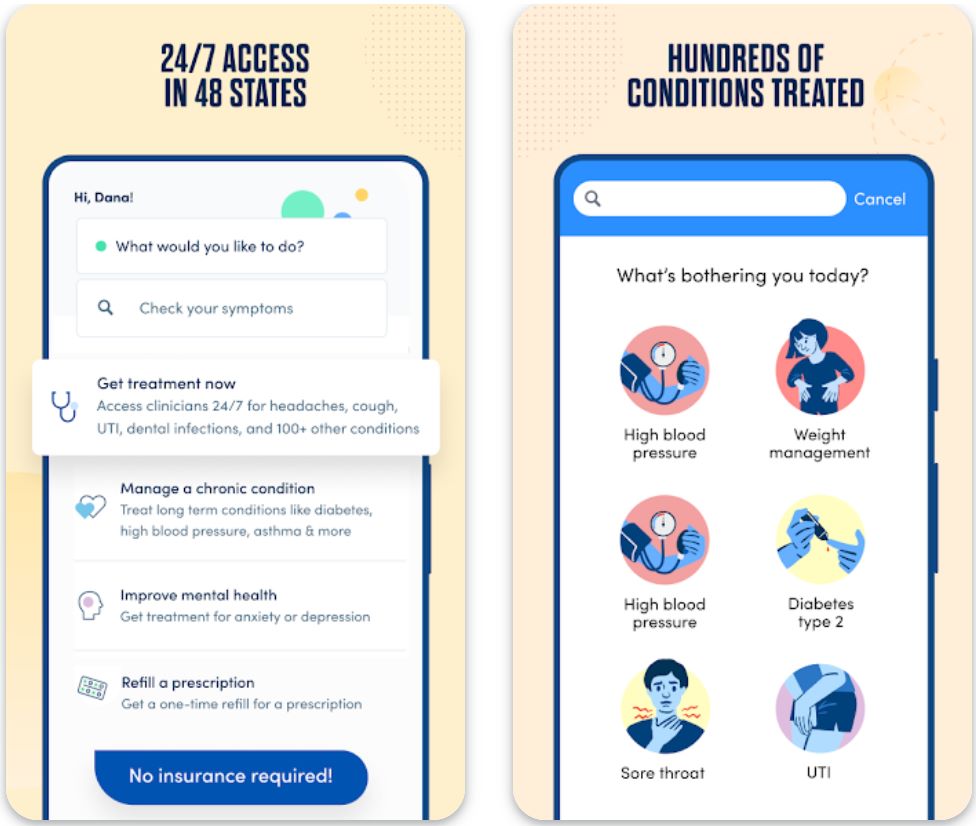
Key Features
Free symptom assessment showing how people like you were diagnosed and treated, powered by millions of anonymized medical records.
Chat, video, or messaging access to licensed clinicians for urgent and primary care whenever you need it.
Remote care and ongoing support for conditions like hypertension, diabetes, and weight management.
Get prescriptions and pharmacy delivery where medically appropriate, directly through the platform.
Large patient record datasets guide care decisions using the "people like you" model for personalized recommendations.
Download or Access Link
User Guide
Download the app from Google Play or App Store, or access via web browser.
Input your symptoms and answer follow-up questions for personalized assessment.
See possible conditions and how others with similar symptoms were treated.
If needed, connect via chat, video, or message for diagnosis, prescriptions, or medical advice.
Schedule follow-ups, get personalized care plans, and monitor your progress over time.
Get approved medications delivered directly to your address.
View previous visits and share reports with outside providers if needed.
Notes & Limitations
- The symptom checker does not provide a definitive diagnosis—results are informative, not medical decisions.
- Accuracy is probabilistic; in clinical vignettes, K Health's top-3 diagnosis match rates were lower than general practitioners.
- Some medical conditions may require physical exams, imaging or lab tests that cannot be provided through telehealth.
- Prescription of controlled substances is limited or prohibited via telehealth in many jurisdictions.
- Service availability is restricted by geography, licensing, and state regulations—some features may not be offered in all areas.
Frequently Asked Questions
Yes, K Health partners with health systems and operates under telehealth and medical regulations in U.S. jurisdictions.
A one-time virtual visit is typically priced around $73, or you can subscribe for unlimited visits (first month $49) then billed quarterly.
While K Health offers primary and chronic care services, it may not fully replace in-person care for complex cases or exams requiring physical tests.
Most services are out-of-pocket; K Health generally does not accept insurance for its virtual visits.
K Health anonymizes and aggregates data used in its AI model, and clinicians access only relevant medical data during consultations. The platform adheres to privacy policies and security regulations.
Heidi Health
Application Information
| Author / Developer | Heidi Health is an Australian health technology company (formerly founded as Oscer) led by Dr. Thomas Kelly. It develops AI medical scribe software to assist healthcare providers in automating clinical documentation. |
| Supported Devices |
|
| Languages / Countries | Heidi is used globally and trusted in 50+ countries. The platform supports multiple specialties, document types, and multiple languages in notes (e.g., therapy notes in patient's preferred language). |
| Pricing Model | Heidi offers a free core plan that supports baseline note generation and transcription. Premium features (e.g., custom templates, "Ask Heidi" assistant, advanced document generation) are available under paid tiers. |
General Overview
Heidi Health is an AI-powered medical scribe platform designed to reduce the administrative burden on clinicians.
It captures clinician–patient conversations in real time (or in offline capture mode), transcribes speech to text, and generates structured clinical notes, referrals, patient summaries, and other healthcare documents. Its tools aim to let clinicians focus more on patient care and less on writing notes.
Heidi is compliant with data privacy standards like HIPAA, GDPR, ISO 27001, and is built for multi-specialty use across various care settings.
Detailed Introduction
In a crowded market of AI scribes, Heidi Health differentiates itself by offering a free entry point and prioritizing clinician adoption over forcing deep EHR integration. The platform is marketed with SEO-relevant terms like "AI medical scribe," "automated clinical documentation," "ambient note generation," and "free AI scribe for clinicians." Heidi's public content (blog posts on using AI scribes safely, tips for setup, compliance statements) supports search visibility around AI in health, medical documentation, and clinician workflow improvement.
Heidi's model allows clinicians to use default note generation immediately, then progressively unlock premium features as they see value. Because documentation style matters, Heidi supports personalized templates to match clinicians' writing voice and workflow.
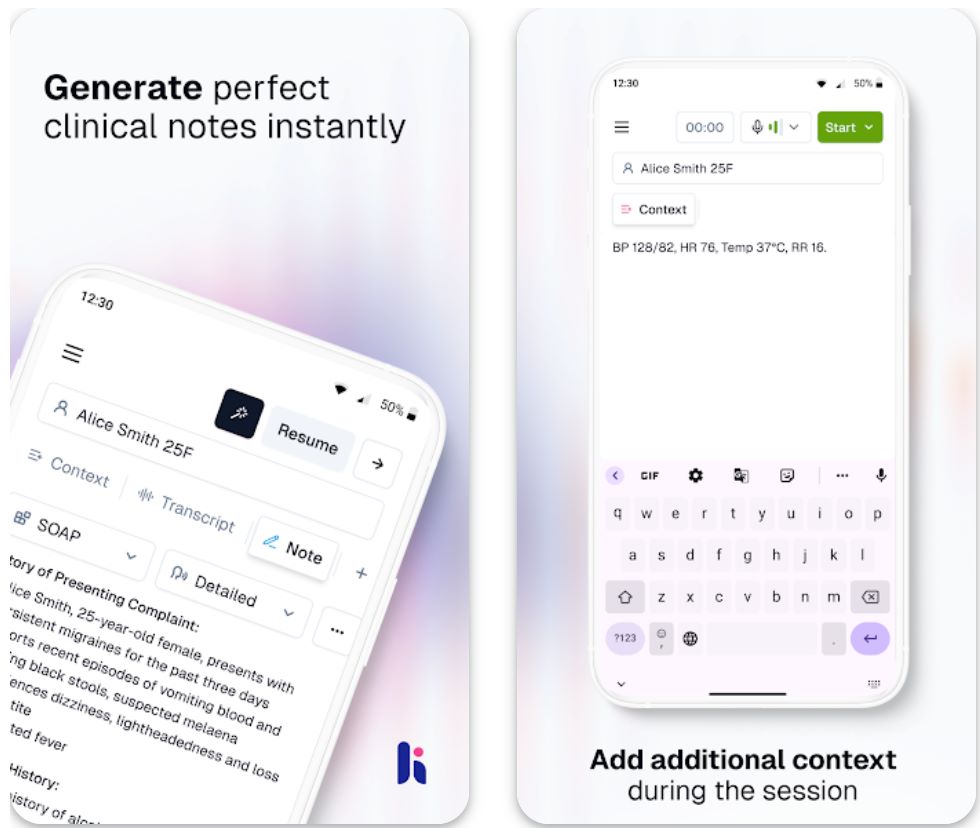
Key Features
Captures consultations in real time or offline audio capture on mobile devices.
Generates clinical notes, referral letters, patient summaries, and assessment reports automatically.
Personalize templates and style to match your unique clinician voice and workflow preferences.
Multi-user collaboration with shared sessions for multiple clinicians working together.
Automatic synchronization across mobile, desktop, and web platforms for seamless workflow.
Fully compliant with HIPAA, GDPR, ISO 27001, and APP standards for data protection.
Download or Access Link
User Guide
Download apps via mobile or desktop, or use the web version directly in your browser.
Create an account with your email and password to get started.
Begin recording a clinician-patient interaction (via mobile or desktop) or upload previous audio files.
Heidi transcribes the conversation and produces structured notes, referrals, and summaries automatically.
Review, edit, add content, and adjust templates or style as needed to match your preferences.
Notes are automatically synchronized across desktop, mobile, and web environments.
If subscribed, unlock custom templates, "Ask Heidi" summarization, and advanced document types.
Important Notes & Limitations
- Mobile app supports offline capture of audio, but structured note generation still needs connectivity.
- EHR integration may be limited or unidirectional; writing back into EHR fields may not always be supported.
- Accuracy depends on audio quality, clarity of speech, and ambient noise; manual review is essential.
- Regulatory and privacy compliance vary by jurisdiction; features or availability may differ in certain regions.
Frequently Asked Questions
Heidi is an AI medical scribe that transcribes clinician–patient conversations and generates structured clinical notes, referrals, summaries, and other documents.
Yes, Heidi offers a free core plan with basic note generation and transcription. Premium features require subscription.
Heidi supports iOS, Android, desktop (macOS/Windows), and web browser access.
On mobile, Heidi can capture audio offline; final note generation syncs when reconnected. On desktop, Heidi requires an active internet connection.
Heidi complies with privacy and security standards including HIPAA, GDPR, ISO 27001, and APP (Australian Privacy Principles), and implements secure data management practices.
Owkin
Application Information
| Author / Developer | Owkin, founded by Dr. Thomas Clozel (MD) and Gilles Wainrib (PhD), is a biotechnology company based in Paris, France. |
| Supported Devices | Web platform (accessible via desktop and laptop). Some internal tools are accessible through secure institutional systems and APIs. |
| Languages / Countries | Available globally, supporting English and other major European languages. Headquarters in Paris with offices in New York, London, and other regions. |
| Pricing Model | Access to core research tools like K Navigator is free for academic researchers; enterprise and pharma features are available through paid partnerships. |
General Overview
Owkin is a pioneering AI-powered biotech company specializing in precision medicine, clinical research, and diagnostics. The platform applies advanced artificial intelligence to biomedical data, helping researchers, clinicians, and pharmaceutical companies accelerate drug discovery and optimize clinical trials.
Owkin leverages federated learning to analyze decentralized patient data while maintaining privacy compliance with standards like GDPR and HIPAA. Through its AI-driven tools, the company enables a collaborative ecosystem that improves disease understanding and therapeutic outcomes in oncology and other medical fields.
Detailed Introduction
Owkin has established itself as a leader in the intersection of AI and life sciences, transforming how medical research and drug development are conducted. The company's proprietary platform integrates multimodal data—including genomics, histopathology images, and clinical information—using federated learning to extract insights from distributed data without moving it.
The company's latest innovation, K Navigator, is an agentic AI co-pilot that assists biomedical researchers in hypothesis generation, data interpretation, and literature exploration. This tool aims to make AI-guided reasoning and pattern recognition accessible to the scientific community.
Owkin also collaborates with major pharmaceutical companies and healthcare institutions to enhance drug development, improve diagnostics, and personalize treatment strategies. Its AI diagnostic solutions, such as MSIntuit CRC (for colorectal cancer) and RlapsRisk BC (for breast cancer), showcase the practical application of AI in clinical settings.
By focusing on data privacy, collaboration, and explainable AI, Owkin stands at the forefront of the global movement toward ethical, data-driven healthcare innovation.
Key Features
Uses multimodal datasets including genomics, pathology, and clinical data for comprehensive analysis.
Ensures data security and privacy across institutions while enabling collaborative AI model training.
AI co-pilot for scientific reasoning, hypothesis exploration, and literature analysis.
Advanced cancer prognosis and treatment optimization solutions including MSIntuit CRC and RlapsRisk BC.
Supports target identification, clinical trial optimization, and therapeutic development.
Connects hospitals, researchers, and pharmaceutical partners worldwide for data-driven innovation.
Download or Access Link
User Guide
Navigate to Owkin's official website to explore available products, solutions, and research tools.
Free for academic researchers. Request access through the K Navigator portal to start using the AI co-pilot for biomedical research.
Contact Owkin for enterprise-level services in diagnostics, drug development, or institutional collaborations.
Implement federated learning frameworks for secure AI modeling with institutional data while maintaining privacy compliance.
Deploy AI diagnostic tools such as MSIntuit CRC and RlapsRisk BC after obtaining regulatory clearance and institutional approval.
Notes and Limitations
- Owkin is primarily designed for institutional and enterprise use, not for individual consumers.
- Diagnostic tools are subject to regulatory approvals (e.g., CE-IVD certification).
- Advanced research and AI modeling features require partnerships or enterprise access.
- Performance depends on data quality and diversity across participating institutions.
- No dedicated mobile application is available for public use.
Frequently Asked Questions
Owkin is an AI-powered biotech company that uses machine learning and federated learning to advance precision medicine, drug discovery, and diagnostics.
Owkin's tools are available to academic researchers, hospitals, and pharmaceutical organizations through partnerships or institutional access.
Some research tools like K Navigator are free for academic users. Enterprise features and AI diagnostic tools require paid licensing or collaboration agreements.
Owkin uses federated learning, allowing AI models to train on local data within hospitals without transferring sensitive information to central servers.
Owkin focuses primarily on oncology (cancer) but also supports broader therapeutic research across biomedical domains.
Lark Health
Application Information
| Author / Developer | Lark Technologies, Inc. |
| Supported Devices | Android, iOS, and compatible health monitoring devices (smart scales, glucose monitors, blood pressure cuffs) |
| Languages / Countries | English; primarily available in the United States |
| Pricing Model | Free for users with eligible health insurance or employer programs; limited access for others |
What is Lark Health?
Lark Health is an AI-powered digital health platform designed to help users prevent and manage chronic conditions such as diabetes, hypertension, and obesity. Through 24/7 conversational AI coaching, Lark delivers personalized support for lifestyle improvements, behavior change, and long-term wellness.
Its clinically validated programs are used by major health plans and employers, helping users monitor their health metrics and receive real-time, data-driven feedback to stay on track toward healthier living.
Detailed Overview
Lark Health stands out in the digital health ecosystem as a fully automated AI health coach that mimics human conversation to guide users toward better health outcomes. The app integrates behavioral science, data analytics, and artificial intelligence to deliver continuous, real-time coaching that adapts to each user's goals and health data.
The platform covers areas like diabetes prevention, hypertension management, weight loss, and behavioral health, offering tailored programs backed by clinical research. By syncing with wearable devices and apps, Lark gathers data on sleep, diet, exercise, and vitals, creating a holistic picture of a user's health. The company partners with leading insurers, making its programs accessible to millions of users without direct cost.

Key Features
Real-time conversational guidance for nutrition, fitness, and wellness improvement tailored to your lifestyle.
Specialized programs for diabetes prevention, hypertension control, and weight management.
Seamlessly syncs with health tracking devices and mobile sensors for automatic data monitoring.
Evidence-based coaching rooted in cognitive behavioral therapy (CBT) principles.
Available through partnered healthcare plans and employers at no additional charge.
Download or Access Link
How to Get Started with Lark Health
Create an account through the Lark Health website or mobile app using your email address.
Confirm if your insurance provider or employer offers Lark programs at no cost to you.
Link compatible health monitoring devices for automatic tracking of vitals, activity, and sleep.
Chat with Lark's AI coach to receive instant feedback and personalized action plans for your health goals.
Review weekly summaries and health insights to stay motivated and informed about your wellness journey.
Important Limitations
- Not suitable for emergency or urgent medical care situations
- Some advanced programs require insurance or employer eligibility verification
- Effectiveness depends on consistent user engagement and accurate data input
- Currently supports English only, limiting accessibility in non-English-speaking regions
Frequently Asked Questions
Lark Health is free for users covered by partnered insurance plans or employer wellness programs. Users without eligible coverage may have limited access to certain features.
No. Lark provides AI-powered coaching and support for lifestyle improvements but does not offer medical diagnosis, treatment, or emergency care. Always consult your healthcare provider for medical decisions.
Lark integrates with most smartphones (Android and iOS), smart scales, fitness trackers, glucose monitors, and blood pressure cuffs. Check the app for a complete list of supported devices.
Lark offers specialized programs for diabetes prevention, hypertension management, weight control, and overall wellness improvement through lifestyle modifications.
Yes. Lark complies with HIPAA regulations to ensure all user data is securely protected, encrypted, and kept confidential. Your health information is never shared without your explicit consent.






No comments yet. Be the first to comment!