AI Empowers Disease Diagnosis from X-ray, MRI, and CT
Artificial intelligence (AI) is becoming a powerful tool in modern medicine, especially in disease diagnosis from X-rays, MRI, and CT scans. With its ability to process medical images quickly and accurately, AI helps doctors detect abnormalities earlier, shorten diagnosis time, and improve treatment outcomes for patients.
Medical imaging is central to diagnosis. X-ray, CT and MRI scans generate vast visual data about the body's internal state.
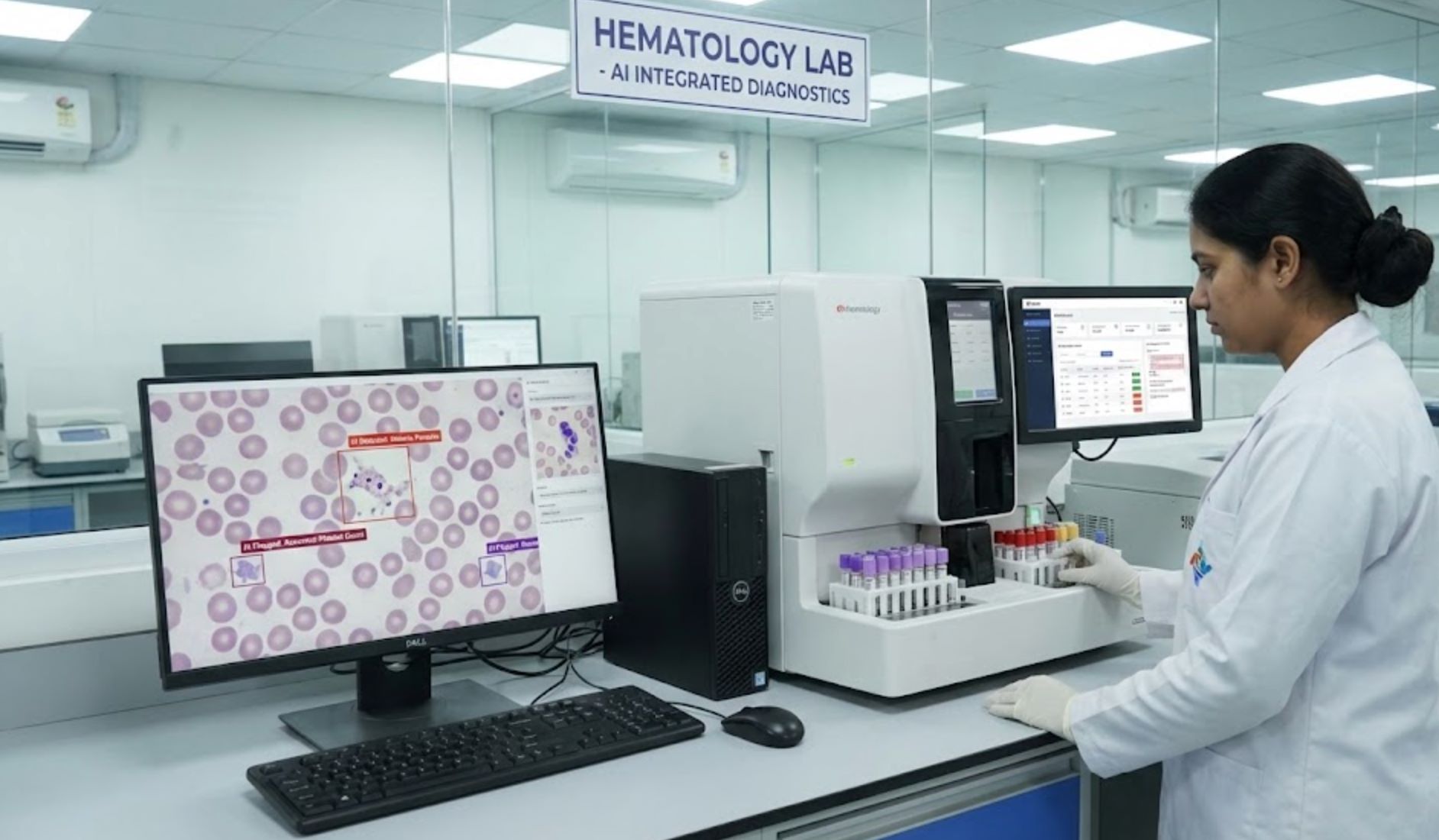
This mismatch arises from the huge workload on radiologists. Artificial intelligence (AI), especially deep learning, can help by automatically "reading" images. Convolutional neural networks trained on large image databases learn to recognize patterns of disease (like tumors, fractures, or infections) that may be subtle or hard to spot. In practice, AI can highlight suspicious areas, quantify abnormalities, and even predict disease.
AI Enhancements in X-ray Imaging
X-rays are the most common diagnostic images – fast, cheap and widely available. They are used to diagnose chest diseases (pneumonia, tuberculosis, COVID-19), bone fractures, dental issues and more.
However, reading X-rays well requires experience, and many places lack enough radiologists. AI can ease the burden.
Deep-learning models like the famous CheXNet have been trained on hundreds of thousands of chest X-rays. CheXNet (a 121-layer CNN) detects pneumonia on chest X-rays with accuracy above practicing physicians.
— Stanford ML Group Research
In orthopedics, AI-driven X-ray analysis can automatically identify subtle fracture lines that may be missed in busy clinics.
Key X-ray AI Tasks
- Detect lung diseases (pneumonia, TB, cancer)
- Identify pneumothorax and fluid
- Spot bone fractures or dislocations
- Screen for COVID-19 or other infections
AI tools can flag these findings instantly, helping prioritize urgent cases.
Clinical Results
In some studies AI matched radiologist performance. For example, CheXNet exceeded the average doctor's accuracy on pneumonia cases. However, tests in real hospitals show limits: one large study found radiologists still outperformed current AI on chest X-rays, achieving higher accuracy in identifying lung findings.

AI Innovations in CT Scanning
CT (computed tomography) produces detailed cross-sectional images of the body and is essential for many diagnoses (cancer, stroke, trauma, etc.). AI has shown great promise on CT scans:
Lung Cancer Detection
Recent AI models can detect and segment lung tumors on CT nearly as well as expert radiologists. A 2025 study used a 3D U-Net neural network trained on a large dataset (over 1,500 CT scans) to identify lung tumors.
Segmentation accuracy almost matching doctors' (Dice scores ~0.77 vs 0.80). AI sped up the process: the model segmented tumors much faster than physicians.
Brain Hemorrhage Detection
In emergency medicine, AI aids rapid stroke care. For instance, the commercial AIDOC algorithm flags intracranial bleeding on head CT.
This can alert doctors to critical bleeds in seconds.
Other CT Applications
- Chest CT for identifying COVID-19 pneumonia patterns
- CT angiography for calcium scoring
- Abdominal CT for detecting liver lesions
- Kidney stone identification
In the lung cancer example, AI-assisted CT could improve treatment planning and follow-up by accurately measuring tumor volume.
Many AI tools are now cleared to help read chest and head CTs. For instance, agencies like CMS have even started reimbursing some AI readouts (e.g. coronary plaque scoring on routine lung CTs).

AI Advancements in MRI Imaging
MRI provides high-contrast images of soft tissues (brain, spine, joints, organs). AI is making MRI faster and smarter:
Ultra-Fast MRI Technology
Traditionally, high-quality MRI scans take time, leading to long waits and patient discomfort. New AI-based reconstruction algorithms (Deep Learning Reconstruction, DLR) drastically cut scan time by predicting missing data.
DLR can make MRI scans "ultra-fast" and the technology may become routine on all scanners.
— Medical Imaging Experts
For example, UK researchers and GE Healthcare used AI to let a low-field (cheaper) MRI machine produce images comparable to a conventional high-field scan. This could make MRI more accessible and reduce patient queues.
Enhanced Image Clarity
AI also improves image quality. By learning the difference between noisy and clear scans, DLR denoises images in real time.
- MRI images are clearer, with fewer motion artifacts even if patients move
- For restless children or trauma patients, faster AI scans reduce the need for sedation
- Real-time noise reduction improves diagnostic confidence
Advanced Disease Detection
In clinical diagnosis, AI excels in MRI analysis. For example, in brain imaging, AI-driven models segment and classify tumors accurately.
- Deep learning can label tumor boundaries in 3D MRI
- Quantify tumor size with precision
- Predict tumor genetics or grade from the image alone
- Find strokes, multiple sclerosis lesions or malformations quickly
- Pinpoint ligament tears or spinal disc problems faster than manual methods
Overall, AI transforms MRI by making scans quicker and data richer.
By integrating patient scans and labelling data, AI enables 3D measurements that support personalized treatment planning. Hospitals experimenting with AI MRI report smoother workflow and more consistent interpretations.

Benefits of AI in Medical Imaging
AI brings several advantages across X-ray, CT, and MRI:
Speed & Efficiency
- AI algorithms analyze images in seconds
- Flag urgent findings (lung opacities, strokes, fractures)
- Enable doctors to prioritize care effectively
- Faster imaging means more patient throughput
In the lung tumor CT study, the AI segmented tumors far faster than manual tracing. Faster imaging (especially MRI) means more patient throughput and shorter wait times.
Accuracy & Consistency
- Match or exceed human accuracy on specific tasks
- Eliminate intra-observer variability
- Consistent marking of findings every time
- Quantitative precision (exact tumor volume)
Models like CheXNet (pneumonia detection) and others have shown higher sensitivity than average radiologists. This quantitative precision aids monitoring and treatment planning.
Extended Expertise
- Acts as expert assistant in underserved regions
- Flags suspected TB or pneumonia in remote clinics
- Expands access to diagnostic care
- Brings imaging insights to areas lacking radiologists
Stanford's CheXNet team notes that expert-level automation could bring imaging insights to underserved areas, addressing the global shortage of radiologists.
Quantitative Insights
- Extract hidden patterns from images
- Predict genetic mutations of tumors
- Forecast patient outcomes from image features
- Enable early disease risk prediction
On MRI, certain AI models predict genetic mutations of tumors or patient outcomes from image features. Combining image analysis with patient data may lead to early disease risk prediction.

Challenges and Considerations
While promising, AI in imaging has caveats:
Performance Variability
AI models may not generalize to every setting. Studies find that some tools perform well in one hospital but worse elsewhere.
This means clinicians must verify AI suggestions and maintain critical oversight of automated recommendations.
Need for Expertise
Radiologists remain essential. Current guidance emphasizes AI as an aid, not a replacement.
- Human oversight ensures subtleties and clinical context are considered
- Integration requires training radiologists to trust and challenge AI findings
- Final diagnostic decisions must incorporate clinical judgment
Data and Bias
AI is only as good as its training data. Image datasets must be large and diverse.
Regulation and Costs
Although many AI tools are cleared (FDA approvals), actually implementing them can be expensive and requires workflow changes.
- Reimbursement models are just emerging (e.g. CMS covers some AI-driven CT analyses)
- Hospitals must consider costs of software, hardware and training
- Workflow integration requires significant planning and resources
Privacy and Security
Using AI involves patient data. Strict safeguards (encryption, de-identification) are vital to protect privacy.
Careful design of AI-aided workflows can boost human performance. In practice, combining the speed of AI with the judgment of clinicians yields the best results.
— Harvard Medical Research Report

Future Outlook
AI in medical imaging is advancing rapidly. Leading companies and research groups continue to improve algorithms.
Foundation Models
"Foundation models" (very large AI networks trained on diverse medical data) may soon provide even broader diagnostic capabilities.
Automation Expansion
We expect more tasks (e.g. full organ segmentation, multi-disease screening) to become automated.
Global Implementation
Collaborative projects aim to leverage AI for public health (e.g. TB screening in low-resource areas).
Internationally, collaborative projects aim to leverage AI for public health (e.g. TB screening in low-resource areas). National health services (like the UK's NHS) are investing in AI-ready scanners to reduce costs.

Key Takeaways
In summary, AI supports disease diagnosis through X-ray, CT and MRI by enhancing accuracy, speed and access.
While radiologists still make the final diagnoses, AI tools help them see more and see faster. As the technology matures, we can expect AI to be an indispensable partner in imaging, improving patient care worldwide.






No comments yet. Be the first to comment!