AI Predicts Heart Disease Risk
Artificial Intelligence (AI) is ushering in a new era of heart disease prevention. By analyzing CT scans, ECGs, and genetic data, AI helps doctors detect early signs of heart attack, heart failure, or sudden cardiac death. Discover leading AI tools like Oxford Heart Scan, Mayo ECG AI, and Scripps Genomic Risk in this article.
Cardiovascular diseases claim approximately 17.9 million lives annually, making them the leading cause of death globally. Early identification of high-risk individuals is crucial for preventing heart attacks and heart failure before they occur.
Traditional risk assessment methods—based on age, cholesterol, blood pressure, and family history—have significant limitations. They often treat patients as statistics, missing subtle personal risk indicators that could signal danger.
Artificial intelligence is revolutionizing cardiac risk prediction by uncovering hidden patterns in medical data that clinicians cannot easily detect. From analyzing medical images for invisible disease markers to processing years of health records, AI algorithms predict heart problems earlier and more accurately than conventional approaches.
- 1. Why Early Detection Matters
- 2. How AI Transforms Cardiac Risk Prediction
- 3. Key Benefits of AI in Cardiac Risk Prediction
- 4. Early Action Saves Lives
- 5. Personalization Drives Engagement
- 6. AI Tools and Applications
- 7. Challenges and Implementation Considerations
- 8. The Future of AI in Cardiac Prevention
- 9. Conclusion
Why Early Detection Matters
Heart disease often progresses silently—many patients experience no symptoms until a catastrophic cardiac event occurs. Early risk identification enables healthcare providers to recommend preventive interventions (lifestyle modifications, medications) before complications develop.
Consider undiagnosed conditions like heart valve disease or reduced cardiac function: patients may feel completely normal while facing significant risk for heart failure or sudden cardiac events. Early detection allows timely treatment to prevent serious outcomes.
This diagnostic gap means many at-risk patients remain unrecognized while others receive unnecessary interventions without benefit. AI addresses this challenge by analyzing complex health data far beyond human capacity, revealing early warning signs of cardiac disease.

How AI Transforms Cardiac Risk Prediction
Artificial intelligence excels at detecting patterns within large, complex datasets—precisely what's needed for superior heart risk prediction. Modern AI neural networks learn from vast medical datasets (images, sensor readings, electronic health records) to recognize features correlating with future cardiac events.
AI identifies subtle factor combinations—many invisible to human analysis—that precede conditions like heart attacks and heart failure. Here are the key applications transforming cardiac risk assessment:
Medical Image Analysis for Hidden Risk Markers
Researchers at the University of Oxford developed an AI system analyzing routine cardiac CT scans to predict heart attack, heart failure, or cardiac death risk up to ten years in advance.
The AI detects artery inflammation by identifying subtle changes in fat tissue surrounding heart vessels—changes invisible to the human eye. These inflammatory signals indicate elevated risk even when arteries appear only mildly narrowed.
Study Scale
Analyzed 40,000 patients
- Tracked 10-year outcomes
- Validated predictions
Clinical Impact
Changed treatment for 45% of patients
- Initiated preventive medications
- Prevented cardiac events
When hospitals implemented AI-generated risk scores, clinicians modified treatment plans for 45% of patients based on newly identified risk. This AI-enhanced analysis provided earlier warnings, enabling interventions to prevent heart attacks and deaths that might otherwise have occurred undetected.
Specialized Heart Imaging for Arrhythmia Risk
Johns Hopkins University researchers created MAARS (Multimodal AI for Arrhythmia Risk Stratification)—a model predicting sudden cardiac arrest risk in patients with hypertrophic cardiomyopathy, a common inherited heart condition.
MAARS combines contrast-enhanced cardiac MRI images with patient medical records to identify scar patterns in heart muscle signaling lethal arrhythmias. These fibrosis patterns—previously indecipherable from raw MRI scans—are precisely detected by AI to assess risk.
Accuracy Rate
- ~50% overall accuracy
- Limited pattern recognition
- High false negatives
Accuracy Rate
- 89% overall accuracy
- 93% for ages 40–60
- Doubled prediction accuracy
The AI model more than doubled accuracy compared to standard approaches. By highlighting problematic scar areas, MAARS helps doctors tailor preventive treatments—determining who truly needs an implanted defibrillator versus unnecessary device surgery.
This AI could "transform clinical care" by saving lives and sparing others from unnecessary device surgeries.
— Johns Hopkins Research Team
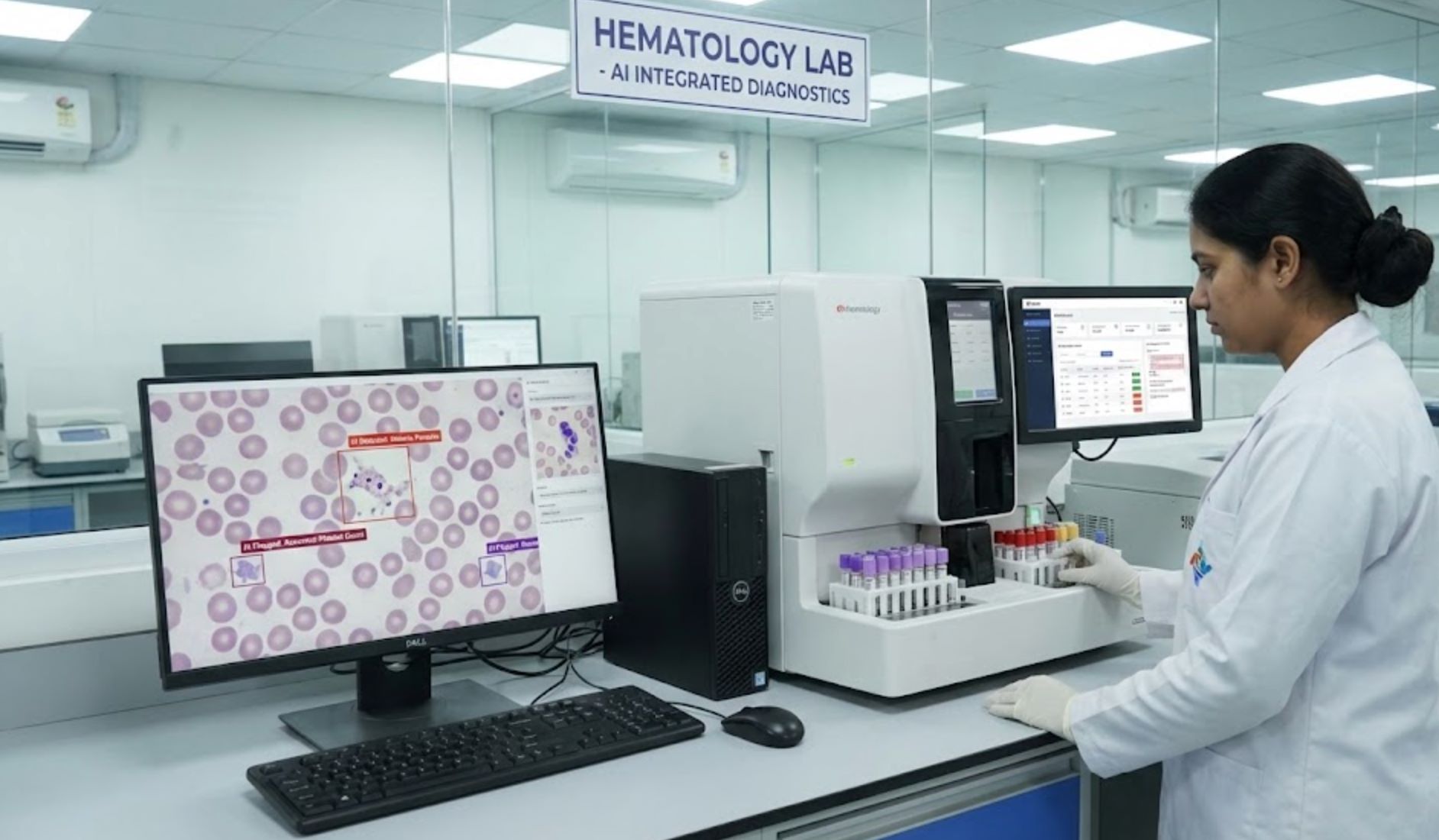
Wearables and Routine Tests Enhanced by AI
AI is making everyday health tools remarkably effective at detecting silent cardiac problems. Mayo Clinic researchers applied AI to routine electrocardiograms (ECGs) and discovered these simple tracings can reveal weak heart pump function before symptoms appear.
Left ventricular dysfunction—a heart failure precursor—often goes unnoticed until severe. Mayo's AI system, trained on over 7 million ECGs, identifies this condition 93% of the time, even when human interpretation reveals nothing obviously abnormal. This accuracy exceeds typical cancer mammogram screening performance.
This AI technology has been adapted into an Apple Watch app, enabling wearable devices to detect weak heart pump function remotely. This low-cost, non-invasive screening allows early heart failure treatment before progression.
AI Stethoscopes
Smartwatch Integration
Early Intervention
These innovations demonstrate how ordinary tests—ECGs, digital stethoscope recordings, smartwatches—become powerful screening tools through AI, identifying at-risk patients who would otherwise be missed.
Big Data Mining: Health Records and Genetics
Beyond images and signals, AI processes vast datasets from electronic health records (EHR) and DNA analysis to refine personalized risk predictions.
Scripps Research scientists in La Jolla, California developed a "meta-prediction" AI model combining traditional risk factors with genomics and long-term health records to predict 10-year coronary artery disease risk. According to lead researcher Dr. Ali Torkamani, this AI approach was twice as effective as standard risk scoring methods at identifying patients who will develop heart disease.
This personalized approach moves beyond one-size-fits-all assumptions (like "all older men are high-risk") toward nuanced assessment where your unique combination of genetics, lifestyle, and health history determines your risk.
As we personalize the risk more and more, that will get people to engage in improving their heart health.
— Dr. Ali Torkamani, Scripps Research
More accurate, personalized predictions motivate individuals to take preventive action when they understand how their specific factors contribute to risk.
Unconventional Data: Eyes, Voice, and Beyond
AI's flexibility enables analysis of almost any health-related data. Remarkably, a simple eye snapshot may reveal cardiovascular risk.
Researchers demonstrated that AI can analyze retinal images (back of the eye) to predict heart attack and stroke likelihood—because tiny eye blood vessels reflect overall vascular health.
In a study of over 1,100 people with diabetes or prediabetes, a deep learning algorithm classified retinal photos into low, medium, and high cardiovascular risk groups. Over 11-year follow-up, those AI-flagged as high-risk were 88% more likely to experience cardiac events than those deemed low-risk—even after accounting for traditional factors like age and blood pressure.
A simple eye exam enhanced by AI could help identify people needing aggressive heart prevention—exemplifying how AI finds meaningful signals in data clinicians don't typically use for cardiology assessment.
Experimental AI systems are also analyzing voice recordings and other novel signals to detect heart failure or artery disease based on vocal markers—an emerging area demonstrating that unexpected data sources may carry telltale disease patterns when examined with AI. These innovations expand the toolkit for assessing heart health through convenient, non-invasive methods.
Key Benefits of AI in Cardiac Risk Prediction
Earlier Detection
AI identifies warning signs years before clinical events occur
- Microscopic inflammation detection
- Faint cardiac abnormalities
- Earlier intervention opportunity
Improved Accuracy
AI dramatically outperforms traditional risk predictors
- Fewer high-risk patients missed
- Reduced false alarms
- Confident decision-making
Personalized Care
Risk assessment tailored to individual characteristics
- Hundreds of unique data points
- Genomic integration
- Enhanced patient motivation
Efficiency & Access
Leverages widely available tests for broad screening
- Primary care integration
- Home-based monitoring
- Reduced healthcare costs
Continuous Learning
AI systems improve with additional data
- Enhanced accuracy over time
- Emerging risk factor detection
- Updated prevention guidelines
Transparency
AI provides reason codes explaining predictions
- Highlighted risk factors
- Doctor-patient understanding
- Shared decision-making
Early Action Saves Lives
In the Oxford study, identifying a patient's elevated 10-year risk enabled preventive medications (statins, anti-inflammatories) to be administered well before any heart attack. Early intervention prevents cardiac events—and AI provides the extended lead time necessary for effective prevention.
Personalization Drives Engagement
Instead of generic risk statements ("you're a 65-year-old male, so risk is high"), AI considers dozens or hundreds of individual data points—your genome, imaging, wearable data, and more. This personalized risk profile motivates patients more effectively. Understanding that poor sleep or subtle ECG changes contribute to your specific risk encourages lifestyle improvements and medication adherence.

AI Tools and Applications
To make this discussion more concrete, let’s look at some real-world AI applications that are already predicting heart disease risk or are on the horizon. These examples underscore how AI is being used by leading institutions and what benefits it brings:
CardioRiskNet
| Developer | CardioRiskNet was developed by academic researchers as part of a biomedical engineering study, published in MDPI Bioengineering (2024). The project involves AI and medical data scientists collaborating on cardiovascular disease (CVD) prediction and prognosis. |
| Supported Devices | Not a mobile app; operates as a research or clinical decision-support system on institutional or research servers. |
| Languages | Available in English only; no multilingual or localized versions documented. |
| Availability | Research-based AI framework with no free or paid plans for general users. |
Overview
CardioRiskNet is an advanced hybrid AI model designed to predict heart disease risk and assist clinicians in cardiovascular prognostics. It integrates clinical, imaging, and genetic data to deliver interpretable predictions on a patient's cardiovascular disease likelihood. Using explainable AI (XAI) techniques, it offers transparency by clarifying why certain risk factors influence outcomes. Early trials demonstrate high accuracy and specificity, highlighting its potential in precision cardiovascular medicine.
Introduction
Cardiovascular disease remains a leading global cause of death, making early risk detection vital for prevention and treatment. CardioRiskNet addresses limitations of traditional risk models that rely on clinical scores or limited data.
This AI framework uses a hybrid learning approach combining machine learning and deep neural networks to analyze diverse patient inputs—demographics, medical history, lab results, imaging biomarkers, and genetics. It employs attention mechanisms to prioritize key variables and explainable AI (XAI) for transparency and interpretability.
Unlike black-box AI systems, CardioRiskNet enables clinicians to trace prediction rationale, boosting trust and clinical usability. Validation tests show predictive accuracy of ~98.7% and specificity near 99%, demonstrating strong clinical potential.
Key Features
Combines machine learning, deep learning, and active learning for robust performance.
Offers interpretable results with feature-importance visualizations.
Processes clinical, imaging, and genetic data for precise predictions.
Achieved ~98.7% accuracy and ~99% specificity in validation datasets.
Uses attention mechanisms to continuously refine predictive capabilities.
Download or Access Link
User Guide
Gather patient datasets including demographic, clinical, laboratory, imaging, and genetic data.
Load data into the CardioRiskNet environment on a research server or simulation platform.
The AI processes inputs through its hybrid network, applying attention-based feature weighting.
Generates predictive outcomes for cardiovascular risk and disease progression.
Analyze visualization dashboards highlighting key features influencing predictions.
Use results to guide early intervention, prevention, and personalized treatment planning.
Notes & Limitations
- CardioRiskNet is a research framework, not a clinical software product.
- No mobile app or consumer interface is currently available.
- Requires complex datasets (imaging, genetics, clinical records), limiting accessibility.
- External validation across diverse populations is limited.
- No free plan; access restricted to research or institutional collaborations.
Frequently Asked Questions
CardioRiskNet predicts cardiovascular disease risk by analyzing clinical, imaging, and genetic data using AI.
No. It is a research-level AI model intended for scientists and healthcare institutions, not a consumer app.
No public version or free plan exists; access is limited to research or medical collaborations.
It integrates explainable AI (XAI) and hybrid learning, delivering both high accuracy and interpretability.
Not yet. It remains under research evaluation and is not approved for widespread clinical deployment.
Mayo Clinic – cardiovascular AI group
| Developer | Mayo Clinic Department of Cardiovascular Medicine |
| Supported Platforms |
|
| Language & Availability | English; primarily used in the United States and global research collaborations |
| Pricing Model | Paid; implemented exclusively in Mayo Clinic's clinical and research settings |
Overview
The Mayo Clinic AI platform for cardiovascular risk prediction is an advanced artificial intelligence system designed to identify hidden signs of heart disease from routine electrocardiograms (ECGs). Using deep learning algorithms, this AI tool detects asymptomatic left ventricular dysfunction, arrhythmias, and other cardiovascular conditions before symptoms appear, enabling early diagnosis, reducing healthcare costs, and improving patient outcomes through predictive analytics integrated directly into clinical workflows.
How It Works
Mayo Clinic's AI-enabled cardiology program combines decades of medical expertise with cutting-edge machine learning research to transform standard ECGs into powerful diagnostic tools. The AI model processes large ECG datasets to identify subtle patterns indicating early-stage heart failure or structural abnormalities. Unlike traditional ECG interpretation, the system continuously learns from new clinical data, improving its predictive accuracy over time.
Currently deployed within Mayo Clinic hospitals and partner institutions, the AI assists physicians in identifying patients requiring further evaluation or intervention. Clinical trials have demonstrated that this approach detects conditions such as low ejection fraction with significantly higher accuracy than standard screening methods.
Key Features
AI-powered ECG analysis detects early left ventricular dysfunction before symptoms arise.
Integrates with single-lead wearable ECG data for continuous remote patient monitoring.
Clinically validated in large-scale trials conducted by Mayo Clinic researchers.
Designed for seamless integration into hospital and research systems to streamline cardiovascular screening.
Access
Getting Started
The AI cardiovascular tools are available through Mayo Clinic's clinical systems and partner institutions.
Connect patient ECG or wearable device data to the Mayo Clinic AI analysis system.
The algorithm automatically analyzes the ECG for markers of heart failure or arrhythmias.
Results are reviewed by physicians who determine appropriate follow-up care.
The system refines its models over time, ensuring improved diagnostic accuracy.
Important Limitations
- Not available for personal or home use
- No free consumer version exists
- Supplements but does not replace professional medical evaluation and diagnostic imaging
- Ongoing validation required for broader global use beyond Mayo-affiliated hospitals
Frequently Asked Questions
The system identifies early signs of left ventricular dysfunction, arrhythmias, and other cardiac abnormalities using ECG data analysis.
No. The tool is currently limited to clinical use within Mayo Clinic and its research partners.
Clinical studies have shown that AI-enhanced ECG screening increases detection of low ejection fraction by up to 32% compared to routine care.
It is primarily deployed within Mayo Clinic facilities but has been used in international research collaborations.
No. The AI acts as a decision-support tool that assists cardiologists by highlighting at-risk patients for further evaluation.
AIRE AI ECG Model
| Developer | University of Oxford, Mayo Clinic, and international research collaborators (AIRE initiative) |
| Supported Platforms |
|
| Language & Validation | English; validated across the United States, Brazil, and the United Kingdom |
| Pricing Model | Paid access for clinical and research institutions only; not available as a public or consumer app |
Overview
The AIRE AI ECG Model is a state-of-the-art artificial intelligence platform that predicts cardiovascular risk directly from standard electrocardiograms (ECGs). Using deep learning and survival analysis, it provides individualized predictions for outcomes including all-cause mortality, heart failure, arrhythmia, and cardiovascular death. Unlike traditional risk calculators, AIRE detects subtle ECG features that reveal underlying heart disease before symptoms appear. Validated on over one million ECGs, AIRE represents a major advancement in preventive cardiology and AI-assisted healthcare diagnostics.
How It Works
Developed through collaboration between Oxford University researchers and the Mayo Clinic, AIRE uses neural networks to interpret ECGs as dynamic predictors of cardiovascular health. The model was trained on 1.16 million ECGs from 189,539 patients and produces a personalized time-to-event survival curve for each patient, estimating their risk of cardiovascular events or mortality over time.
The model is biologically interpretable—linking specific ECG features to known physiological and genetic pathways related to heart structure and function. This makes AIRE not just predictive but also explainable, a key step in clinical AI transparency. In clinical validation, AIRE outperformed conventional statistical models for predicting heart disease outcomes, offering physicians a faster and more accurate way to identify at-risk patients during routine ECG screening.
Key Features
Predicts all-cause mortality, cardiovascular death, heart failure, and arrhythmias from a single ECG.
Generates individualized time-to-event risk curves for each patient to guide clinical decision-making.
Tested across multiple international populations for generalizability and clinical reliability.
Provides explainable insights connecting ECG features to heart function and physiological pathways.
Designed for seamless integration into hospital and clinical diagnostic systems.
Access & Download
Getting Started
Available through approved research and clinical institutions partnered with the AIRE program.
Input a standard 12-lead ECG or compatible digital recording into the AIRE AI analysis interface.
The model processes the ECG and produces a personalized survival curve predicting the likelihood of cardiovascular events.
Clinicians use the generated report to guide patient management, screening, and preventive care decisions.
The system continuously learns from new patient data to improve predictive accuracy over time.
Important Limitations
- Not available for public or consumer use
- No free version available
- Requires integration with ECG data systems
- Requires professional medical oversight
- Clinical deployment under evaluation in ongoing NHS and academic trials
Frequently Asked Questions
AIRE predicts individual cardiovascular risks—such as heart failure, arrhythmia, or death—based on routine ECG data. It provides personalized risk assessments to help clinicians identify at-risk patients during routine screening.
Studies published in Nature Medicine and peer-reviewed journals demonstrate that AIRE predicts risk outcomes more accurately than traditional statistical models. The model was validated on over one million ECGs for robust clinical reliability.
No. AIRE is designed exclusively for clinical and research use by hospitals and licensed medical professionals. It is not available as a public or consumer application.
AIRE provides time-to-event survival analysis and biologically interpretable insights, rather than simple binary risk classification. This explainability makes it more transparent and clinically actionable for healthcare providers.
The model is under evaluation in healthcare systems including the NHS in the United Kingdom and academic hospitals in the United States and Brazil as part of ongoing clinical trials.
Echo
| Developer | Ultromics, academic research groups, and AI/medical imaging companies specializing in echocardiography |
| Supported Platforms |
|
| Language & Availability | English; primarily deployed in hospitals across the UK, US, and Europe |
| Pricing Model | Paid platform for clinical and research use; no free consumer version available |
Overview
AI echocardiography analysis tools leverage advanced machine learning to automatically assess heart ultrasound images for early cardiovascular disease detection. These platforms automate cardiac measurements, interpret complex imaging patterns, and quantify cardiac function with precision. By identifying structural abnormalities and risk indicators, they enable clinicians to detect heart failure, valvular disease, and other cardiac conditions earlier, improving diagnosis accuracy, treatment planning, and patient outcomes.
How It Works
Echocardiography is the gold standard for evaluating cardiac structure and function, but traditional interpretation requires expert clinicians and is subject to variability between observers. AI-assisted echo platforms address these challenges by automating critical analysis tasks:
- Automatically segment cardiac chambers and quantify ejection fraction
- Assess wall motion and measure global longitudinal strain
- Generate predictive risk assessments linked to future adverse events
- Reduce analysis time and improve consistency across exams
By integrating AI algorithms directly into echocardiography systems, these tools provide both immediate clinical insights and long-term prognostic value for screening and ongoing patient management.
Key Features
AI-powered segmentation and quantification of cardiac chambers and ejection fraction with minimal manual input.
Predictive scoring for cardiovascular outcomes based on echocardiographic biomarkers and AI analysis.
Reduced inter-observer variability and faster analysis through standardized AI-assisted annotations.
Seamless integration with hospital imaging systems for early detection of heart failure, valve disease, and structural abnormalities.
Access
Getting Started
Perform standard echocardiography using compatible ultrasound machines following clinical protocols.
Load echocardiographic images into the AI analysis platform for processing.
The AI tool automatically segments heart structures, measures cardiac function, and identifies abnormalities.
The system generates predictive scores and risk stratification for cardiovascular outcomes.
Cardiologists review the AI-generated report alongside clinical findings to guide patient management decisions.
Important Considerations
- Requires high-quality echocardiographic images for accurate AI analysis
- Ongoing external validation across diverse patient populations
- Paid platform; no free version available
- Implementation may require staff training and system integration support
- Not suitable for home or consumer use
Frequently Asked Questions
These tools can detect heart failure, valvular disease, structural abnormalities, and predict future cardiovascular events based on echocardiographic biomarkers and AI analysis patterns.
No. AI echocardiography platforms are designed exclusively for clinical use in hospitals and research centers. They require professional ultrasound equipment and trained operators.
AI automates precise measurements, reduces human error and observer variability, and analyzes subtle imaging patterns that may be missed during visual inspection alone, resulting in more consistent and reliable assessments.
No. AI echocardiography platforms are paid solutions used in clinical and research settings. There is no free consumer version available.
No. AI serves as a decision-support tool to assist clinicians by automating routine measurements and highlighting potential abnormalities. Professional medical judgment and clinical expertise remain essential for patient care and treatment decisions.
Challenges and Implementation Considerations
While AI's potential in cardiac risk prediction is substantial, important challenges require attention:
Validation Across Diverse Populations
AI models perform only as well as their training data. If datasets lack diversity, AI may not perform equally across all populations.
Researchers emphasize comparing AI tools against established methods (existing risk scores, calcium scans) to confirm genuine improvement. Many research AI algorithms remain preliminary—peer-reviewed studies and regulatory approvals are necessary before clinical integration.
Clinical Workflow Integration
Developing excellent AI models is one challenge; implementing them in daily clinical practice is another. Healthcare systems require user-friendly software integrating AI insights into clinical workflows—for example, medical record alerts flagging at-risk patients.
This integration demands IT investment and clinician training to interpret and act on AI results. Technology adoption often faces resistance, making clear evidence of benefit essential for driving acceptance.
We have the technology pieces, but the next challenge is implementation in clinical settings and patient adoption.
— Dr. Ali Torkamani, Scripps Research
Patients also need to understand and trust AI-driven risk predictions. Effective communication and AI-driven visualizations help people grasp personalized risk. As success stories accumulate, acceptance will grow.
Ethical and Privacy Safeguards
AI's data requirements raise privacy concerns. Medical AI models often train on millions of patient records—strict de-identification and appropriate consent are essential.
AI as Clinical Support, Not Replacement
AI is a tool supporting clinicians, not replacing them. Human expertise remains essential for interpreting AI findings in context and discussing results with patients.
Mayo Clinic emphasizes that AI in cardiology complements physician knowledge and frees time for patient care. The best outcomes combine AI's data-crunching ability with physician clinical judgment and compassion.

The Future of AI in Cardiac Prevention
The future of AI in heart disease risk prediction appears exceptionally promising. AI is becoming a standard component of cardiology evaluation—your annual physical may soon include AI analysis of voice patterns, smartwatch data, ECGs, and ultrasound, synthesized into a personalized heart health report.
Large technology companies and healthcare institutions are investing heavily in this space, driving rapid innovation. As these tools integrate into clinical practice, we can expect:
- Widespread AI screening preventing most preventable cardiac events
- Early detection enabling intervention before symptoms develop
- Personalized prevention strategies based on individual risk profiles
- Reduced emergency hospitalizations through proactive management
- Better healthcare resource allocation to those with greatest need
The vision is a world where far fewer heart attacks and strokes take people by surprise, because AI algorithms will have provided early warnings enabling timely intervention. As heart research leaders express, harnessing AI's power will "prevent countless unnecessary heart-related deaths" through enabling proactive care.
Conclusion
AI is proving to be a transformative ally in combating heart disease. By predicting cardiac risk with unprecedented accuracy—whether through imaging analysis, wearable integration, or big data processing—AI empowers both doctors and patients to take proactive heart health measures.
These technologies, driven by rigorous research from leading global institutions, are steadily transitioning from laboratories and clinical trials into real-world practice. As implementation accelerates, they hold tremendous potential to save lives, personalize care, and establish a new era of preventive cardiology where heart health is maintained with intelligent technological support.






No comments yet. Be the first to comment!