AI Detects Early Cancer from Images
The application of artificial intelligence (AI) in medicine is making a breakthrough in early cancer detection from medical images. With its ability to analyze data quickly and accurately, AI helps doctors identify subtle abnormalities that the human eye might miss. This not only improves diagnostic accuracy but also increases patients’ chances of successful treatment.
Do you want to know how AI detects cancer early from images? Let's find out more details with INVIAI in this article!
By training deep learning models on thousands of annotated scans and slides, AI can learn patterns that even expert clinicians might miss. In practice, AI tools analyze images like mammograms, chest CTs, X-rays, MRIs, ultrasound and pathology slides, flagging suspicious areas and quantifying risk.
AI in cancer care is "an unprecedented opportunity" to improve diagnosis and treatment.
— Medical experts in oncology
For example, an AI-enhanced ultrasound helped one patient avoid an unnecessary thyroid biopsy by showing her lump was benign, demonstrating the practical benefits of this technology in real clinical scenarios.
- 1. How AI Analyzes Medical Images
- 2. Breast Cancer Screening
- 3. Lung Cancer Screening
- 4. Skin Cancer (Melanoma)
- 5. Cervical Cancer Screening
- 6. Colon and Rectal Cancer Screening
- 7. AI in Pathology and Other Imaging
- 8. Benefits of AI in Early Detection
- 9. Challenges and Considerations
- 10. Future Directions
- 11. Conclusion
How AI Analyzes Medical Images
AI systems for imaging typically use deep learning (especially convolutional neural networks) trained on vast datasets. During training, the algorithm learns to extract features like shapes, textures, and colors that distinguish cancerous from healthy tissue.
Training Phase
AI models learn from thousands of annotated medical images, identifying patterns that distinguish cancerous from healthy tissue.
Analysis Phase
The trained AI scans new images and highlights patterns that match learned cancer features with colored boxes and alerts.
Risk Assessment
AI algorithms predict future cancer risk from single images, allowing doctors to personalize screening intervals.
In effect, the AI becomes a super-sensitive "second reader," pointing out subtle lesions that a human might overlook. For instance, an AI reviewing a mammogram or CT slice may mark tiny calcifications or nodules with colored boxes and alerts for the radiologist to inspect.

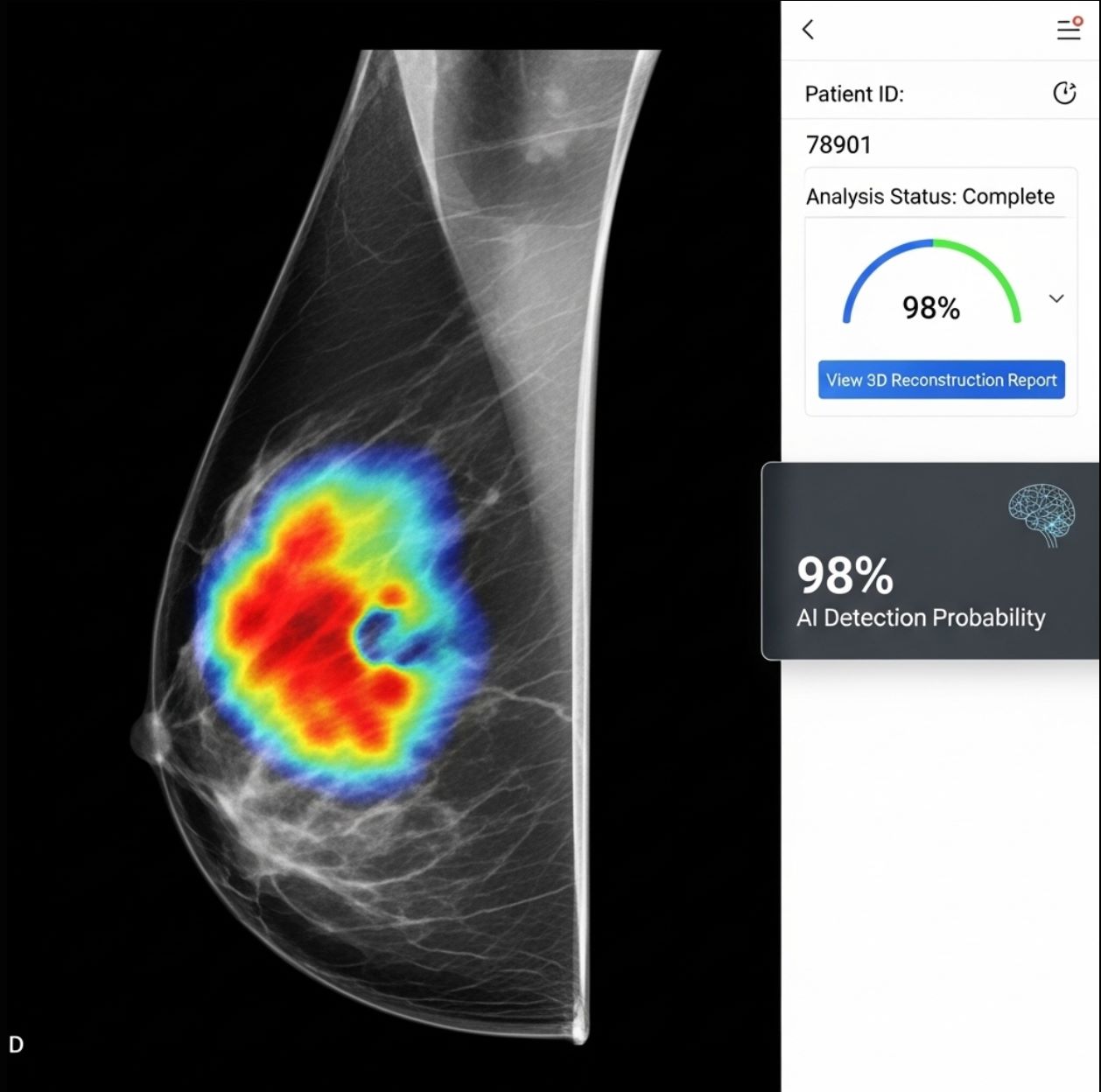
Breast Cancer Screening
Mammography is a prime example where AI is making an impact. Studies show AI support can significantly improve breast cancer detection in screening programs worldwide.
Traditional Method
- 5.7 cancers detected per 1,000 women
- Higher recall rates (false alarms)
- Potential for missed subtle findings
AI-Enhanced Method
- 6.7 cancers detected per 1,000 women
- Reduced recall rates
- Enhanced detection of subtle patterns
AI Capabilities in Mammography
Enhanced Detection
Improves sensitivity and specificity in breast cancer detection.
- Identifies subtle findings
- Predicts invasive potential
Subtle Pattern Recognition
Flags tiny clusters and asymmetries easily missed during routine screening.
- Microcalcifications detection
- Tissue asymmetry analysis
Workflow Optimization
Reduces workload and variability between radiologists.
- Pre-screens images
- Prioritizes suspicious cases
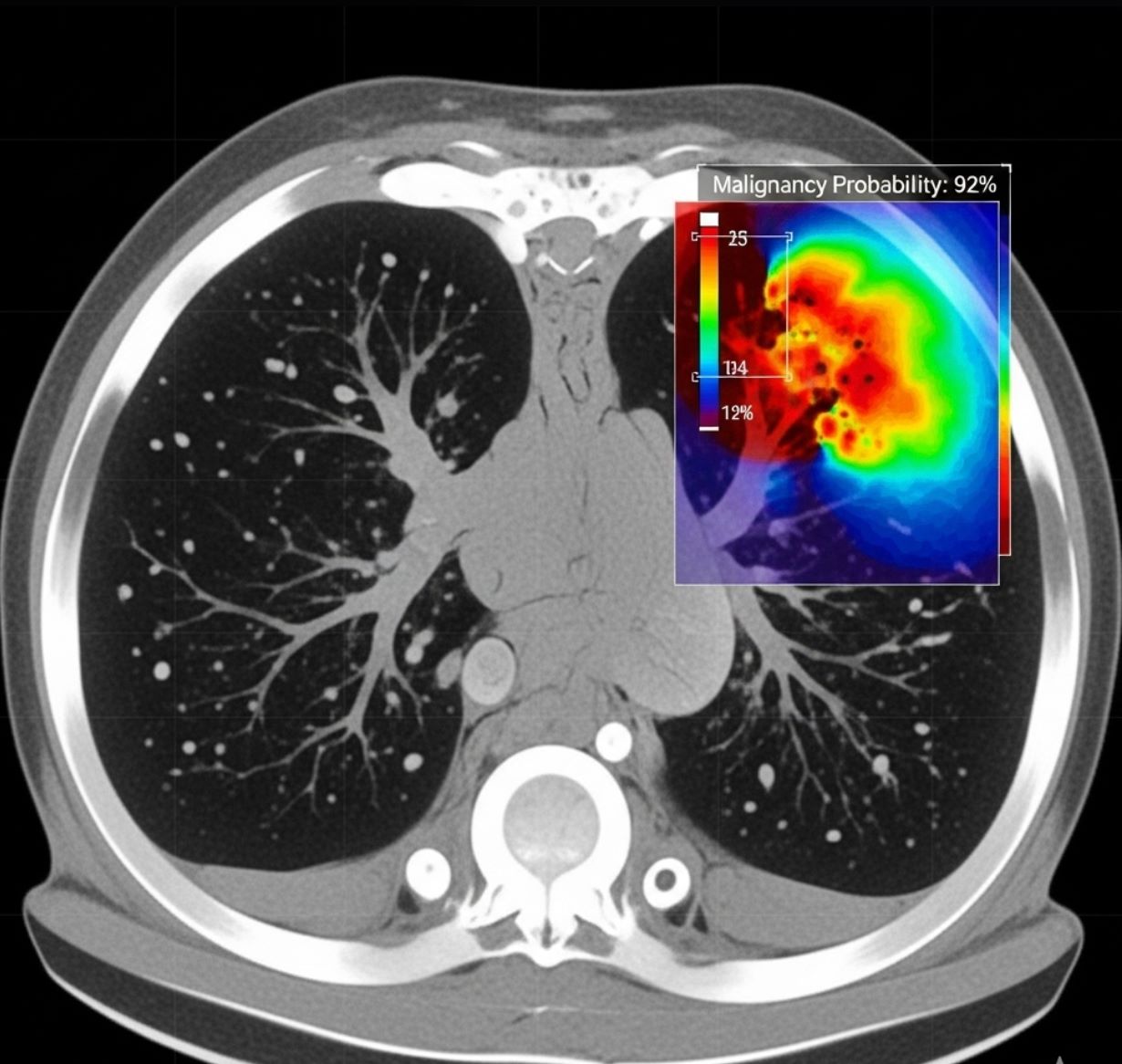
Lung Cancer Screening
AI is also being applied to lung cancer detection on medical images. Low-dose CT (LDCT) scans are used to screen high-risk smokers; AI can enhance this by improving image quality and lesion detection.
Dose Reduction
Automated Detection
Recent models show high sensitivity for both benign and malignant lung nodules, with research systems detecting >90% of nodules on test scans. The U.S. FDA has approved AI tools to assist lung cancer screening, recognizing their role in earlier diagnosis.
AI may also help personalize screening by combining imaging with patient data, allowing algorithms to stratify who needs more frequent scans based on individual risk profiles.
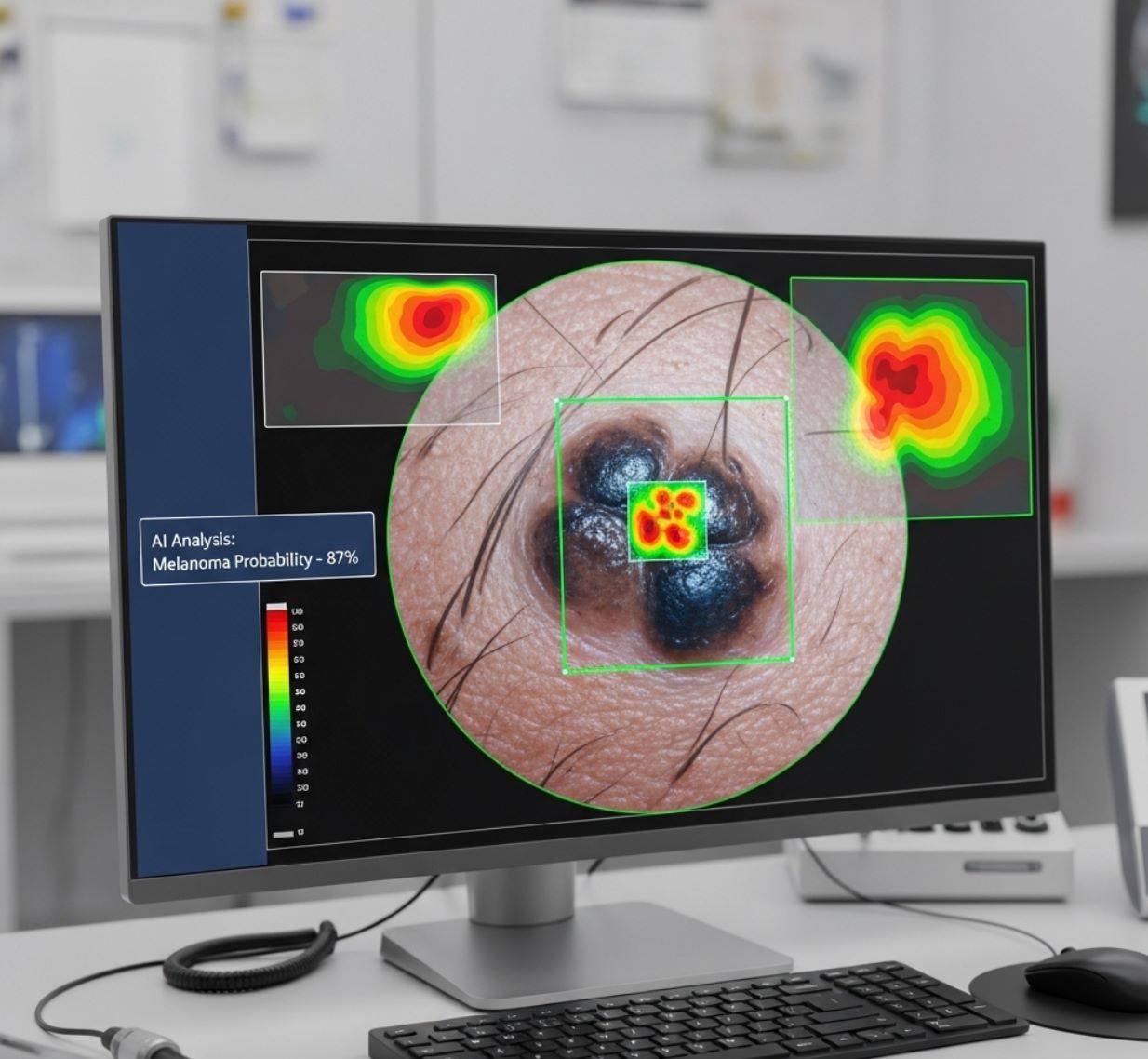
Skin Cancer (Melanoma)
Dermoscopic imaging (magnified skin photos) is another area where AI shines. State-of-the-art deep learning models trained on tens of thousands of skin lesion images can classify moles as benign or malignant with high accuracy.
Stage I Melanoma
- 98% 5-year survival rate
- Minimal treatment required
Advanced Melanoma
- Significantly lower survival
- Extensive treatment needed
AI tools are even being packaged into phone apps or devices that evaluate a photographed mole and estimate its risk, potentially expanding early detection to primary care settings and making screening more accessible worldwide.
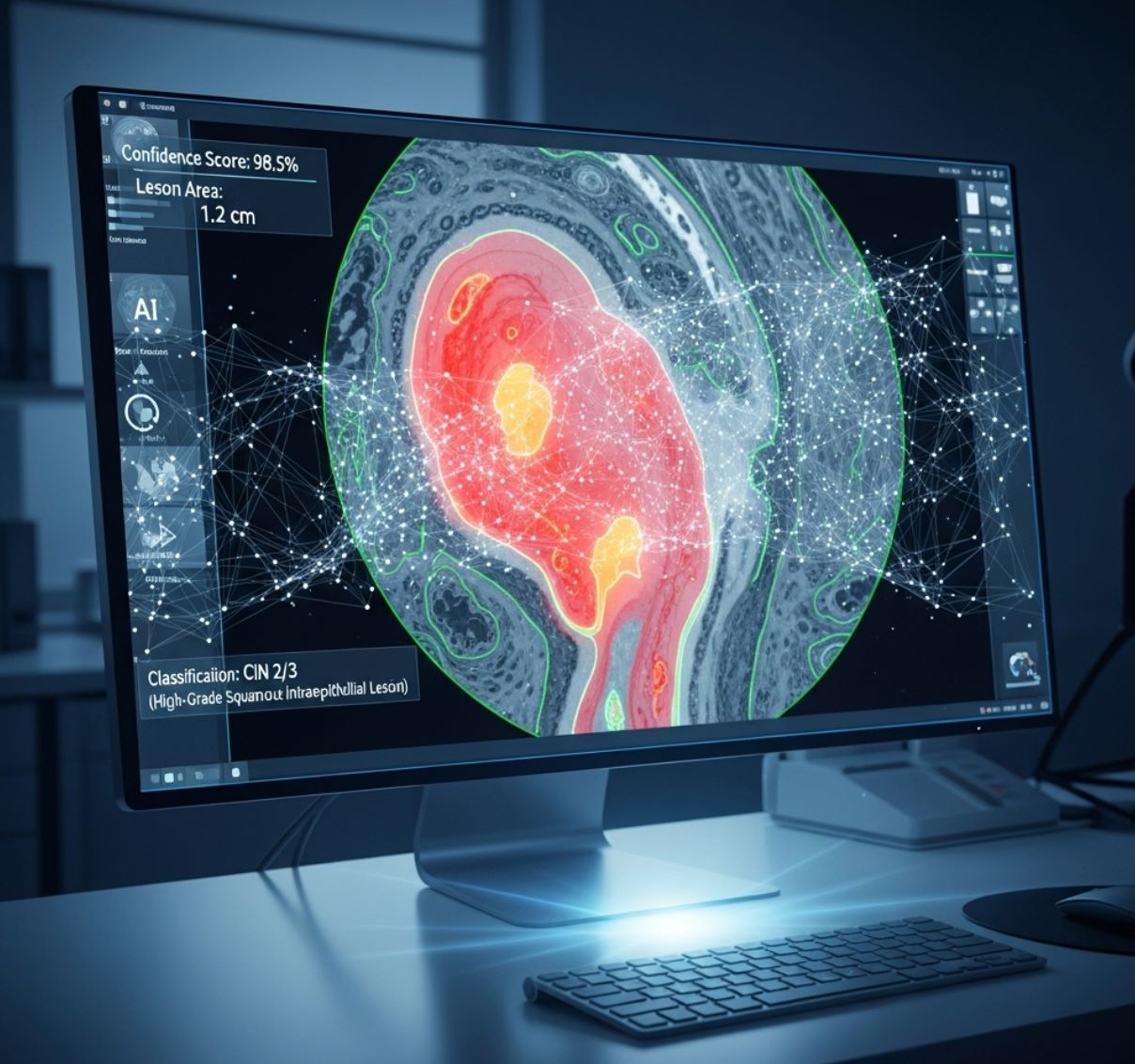
Cervical Cancer Screening
AI is improving cervical cancer screening by analyzing digital images of the cervix. For example, the CerviCARE system uses deep learning on "cervicography" photos (colposcopy-like images) to distinguish precancerous lesions.
High Sensitivity
High Specificity
This kind of AI works alongside traditional Pap smear and HPV testing to catch disease early. The NCI also notes ongoing research on AI for automating precancer detection in cervical screening programs.
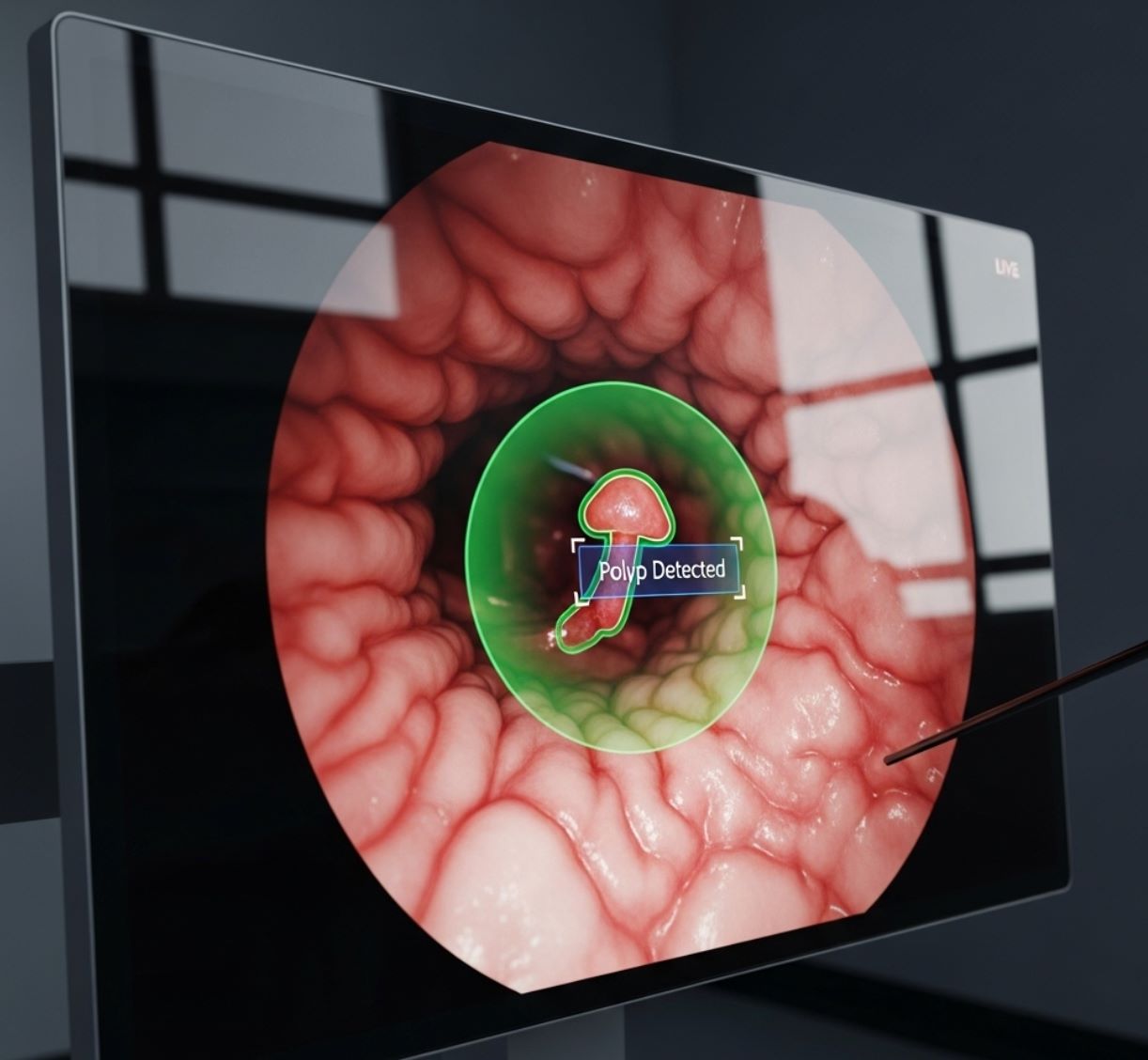
Colon and Rectal Cancer Screening
During colonoscopy, AI assists in real time. Modern systems continuously analyze the video feed from the colonoscope. When the camera images a polyp or suspicious tissue, the AI highlights it on screen (often with a colored box and an audible alert) to grab the doctor's attention.
Increased Detection
Studies show AI increases total polyps detected, especially small adenomas.
- Catches overlooked lesions
- Reduces fatigue-related misses
Quality Consistency
Provides uniform analysis and reduces variability between doctors.
- Consistent "second eye"
- FDA-cleared CADe systems
In other words, AI is excellent at pointing out lots of little lesions, but whether it improves finding the most dangerous pre-cancers is still under review. Even so, an AI "second eye" can reduce fatigue-related misses and lower variability between doctors. The FDA has cleared AI systems (CADe) for clinical colonoscopy to assist endoscopists in polyp detection.
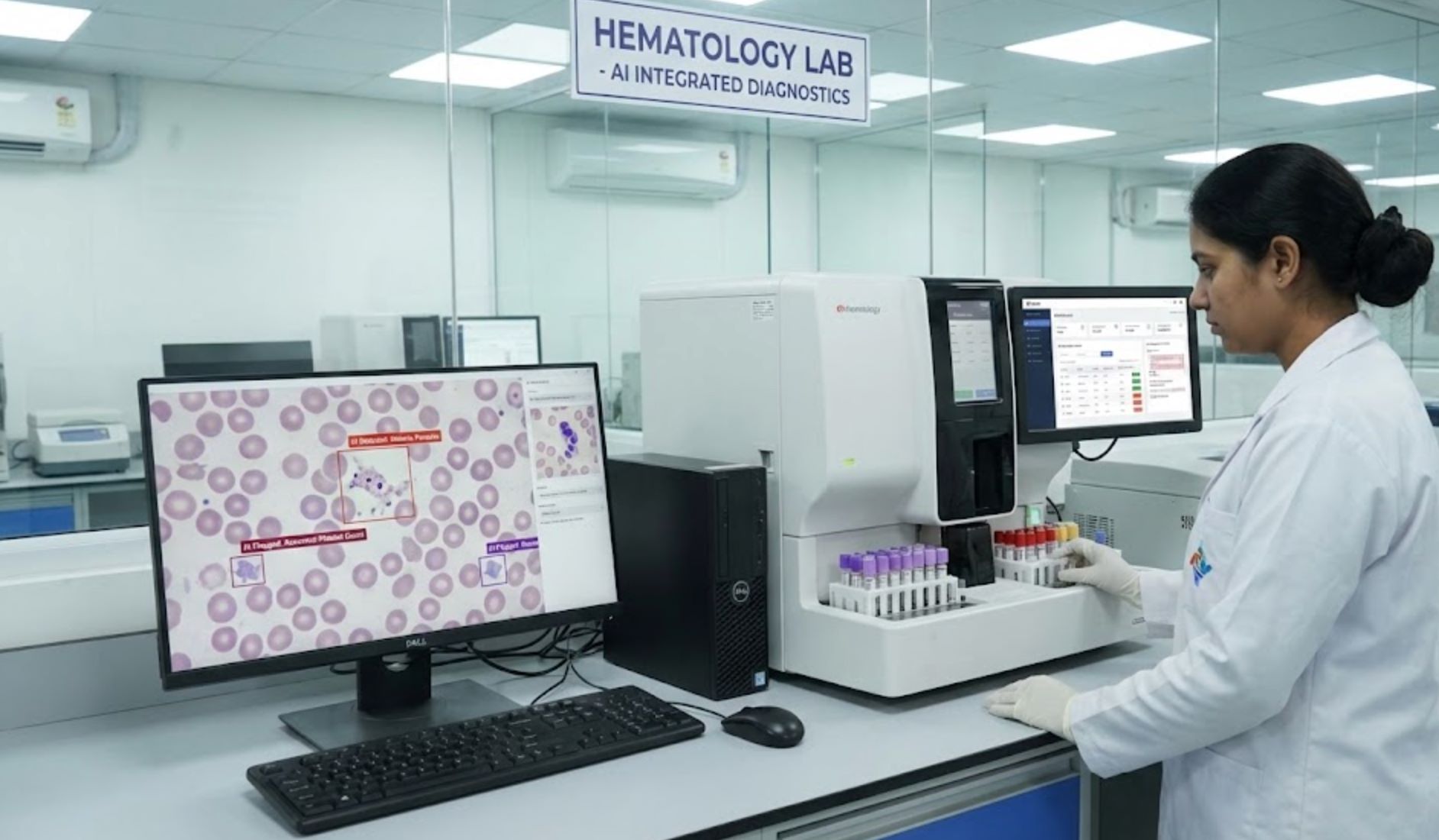
AI in Pathology and Other Imaging
AI's reach goes beyond live imaging to pathology and specialized scans. Digital pathology slides (high-resolution scans of tissue biopsies) are being read by AI algorithms with remarkable precision.
CHIEF AI System
FDA-Approved AI Applications
- AI software for highlighting cancer regions in prostate biopsy specimens
- Brain tumor MRI interpretation systems
- Thyroid nodule ultrasound analysis tools
- Digital pathology slide analysis across multiple cancer types
In short, AI is becoming a versatile assistant: from MRI/CT scans to X-rays to microscope slides, it flags abnormalities that warrant attention, helping pathologists focus on critical areas and improving diagnostic accuracy.

Benefits of AI in Early Detection
Across applications, AI offers several key advantages for catching cancer early, transforming how medical professionals approach screening and diagnosis:
Higher Sensitivity
AI detects very subtle signs that humans might miss.
- 20-40% of interval cancers caught retrospectively
- Earlier detection than human readers alone
Accuracy & Efficiency
Fewer false negatives and sometimes lower false positives.
- Higher positive predictive value
- Faster image processing
Consistent Quality
Uniform analysis without fatigue or distraction.
- Reduces variability between radiologists
- Maintains consistent performance
Preventing Unnecessary Procedures
Global Access
AI-powered approaches can enhance clinicians' ability to evaluate cancers efficiently and accurately. In many trials, combining AI with doctors' expertise outperforms either alone, much like consulting a knowledgeable colleague.
— Medical AI researchers

Challenges and Considerations
AI also brings challenges that must be carefully addressed to ensure effective and equitable implementation across diverse patient populations.
Image Quality Issues
False Alarm Risk
Implementation Challenges
- Hospitals need validated, FDA-approved software and comprehensive staff training
- Regulatory and liability questions about responsibility if an AI misses a cancer
- Integration into existing clinical workflows requires careful planning
- Ongoing trials and post-market studies essential for outcome validation
AI is a tool, not a replacement. Using AI is like "asking a brilliant colleague for input".
— Radiologist perspective on AI integration

Future Directions
The future of AI in cancer detection is promising, with revolutionary developments on the horizon that could transform personalized medicine and screening approaches.
Foundation Models Revolution
Multi-Modal AI Integration
Personalized Screening
Combining imaging with genetic and clinical data for ultra-personalized screening approaches.
- Individual risk stratification
- Customized follow-up intensity
Predictive Analytics
AI could predict not just if cancer is present, but how aggressive it will be.
- Tumor behavior prediction
- Treatment response forecasting
Older AI Systems
- "Primitive" compared to today's models
- Limited scope and accuracy
Advanced AI Systems
- Sophisticated neural architectures
- Multi-modal integration capabilities
Global Validation Studies
International studies (like multicenter trials in Europe and the US) are underway to validate AI tools at scale. As data accumulates, AI will learn from real-world results, continually refining its accuracy through:
- Large-scale multicenter validation trials
- Real-world performance monitoring
- Continuous learning from clinical outcomes
- Cross-population effectiveness studies

Conclusion
In summary, AI is already helping doctors detect cancers earlier from medical images – from mammograms and CT scans to skin photos and biopsy slides. While challenges remain, cutting-edge research and regulatory approvals suggest a future where AI is a standard ally in cancer screening.






No comments yet. Be the first to comment!